Avalere Analysis: Cost-Sharing Reductions Unevenly Applied Across Services in Exchange Plans
Summary
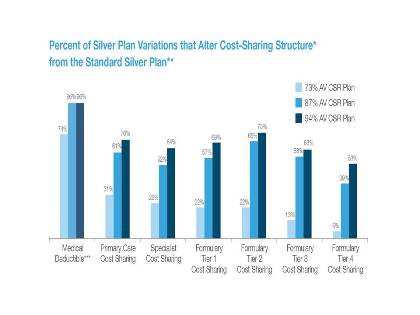
A new analysis from Avalere Health finds that consumers in exchanges receiving federal assistance to reduce their out-of-pocket costs may experience inconsistent reductions in spending depending on the plan they choose.Specifically, the data show broad differences in how issuers amend plan designs to meet cost- sharing requirements for those receiving cost -sharing reductions (CSR). While almost all plans reduce deductibles and out-of-pocket caps in CSR plans, many plans do not lower cost-sharing for other treatments and services, particularly specialty drugs.
“Many people assume that the lowest-income exchange enrollees will have reduced cost-sharing across all services, but the reality is quite different,” said Caroline Pearson, vice president at Avalere. “While all plans must have reduced out-of-pocket limits for individuals earning less than 250 percent of poverty, how consumers will reach those limits differ significantly. For example, consumers may not experience reduced cost-sharing amounts for drugs or physician visits in many plans.”
All carriers that offer silver plans on the exchange must also offer silver CSR variations that have higher actuarial values (AV) for people who qualify for cost-sharing assistance. Individuals with incomes between 100% and 150% of the federal poverty line (FPL) receive the biggest reductions in likely out-of-pocket costs. Beyond requirements to lower maximum out-of-pocket caps , plans have broad discretion in how they meet the AV targets for CSR plans.
Notably, the vast majority-96% of 94% and 87% AV CSR plans-reduced deductibles to help meet new requirements. However, wide variation even exists among carriers that lowered deductibles. For example, the highest deductible ($700) among 94% AV plans analyzed is three times greater than the average ($220).
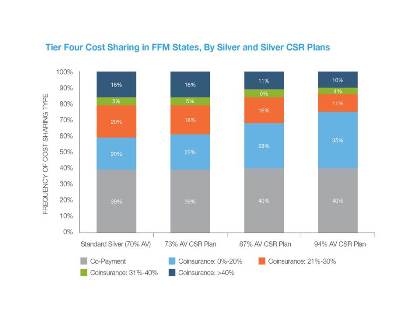
By contrast, a far smaller percentage of plans-including only 5% of 73% variations-reduced cost sharing for Tier 4 medications (specialty drugs). Indeed, a quarter of the 94% AV plans (the plans providing the highest level of cost-sharing assistance) had coinsurance of greater than 20% on the specialty tier.
Notably, Avalere also found that average maximum out-of-pocket limits in CSR plans are lower than those required by the Affordable Care Act. Specifically, among 87% AV CSR plans, the average out-of-pocket limit is $450 (or 20%) lower than required, while among 94% AV CSR plans, the average out-of-pocket maximum is $1,140 (or 22%) less.
“Issuers will continue to have flexibility in how they design cost sharing reduction plans in 2015,” said Dan Mendelson, CEO and founder of Avalere Health. “Looking ahead, consumers who qualify for cost-sharing reductions should look closely at how the plan benefit is structured because it could have a major impact on their actual out-of-pocket costs.”
This analysis was funded by PhRMA. Avalere maintained editorial control over the content of the analysis and release.
Methodology
:
Avalere analyzed the 11th version of the Department of Health and Human Services (HHS) Landscape file available on HealthCare.gov. The file contains details on individual and family premiums and benefit designs for plans across the 34 states in the Federal Facilitated Exchange (FFE). The 34 states in the federally-facilitated marketplace include: Alaska, Alabama, Arkansas, Arizona, Delaware, Florida, Georgia, Iowa, Illinois, Indiana, Kansas, Louisiana, Maine, Michigan, Missouri, Mississippi, Montana, North Carolina, North Dakota, Nebraska, New Hampshire, New Jersey, Ohio, Oklahoma, Pennsylvania, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, West Virginia, and Wyoming. This analysis focuses solely on this data file and, therefore, does not reflect plans offered in any state-based exchange.
The file contains 5,800 total silver plans, including standard silver plans as well as the required “silver plan variations.” Drug coverage data in the HHS Landscape file are structured into four formulary tiers; therefore, for plans that have fewer or more than four formulary tiers, the data in this file may not align with the plan’s true formulary structure. The accuracy of all analysis is limited by the accuracy of the data included in the Landscape file itself.
Although Avalere analyzed and included a number of details about deductibles, we did not consider whether a person needs to meet a deductible when analyzing cost-sharing categories to conduct our analysis (e.g., if coinsurance is 10% after meeting a $1,000 deductible, when analyzing costs for the service, Avalere used the 10% coinsurance amount). Plans that noted that there was no charge, or no charge after the deductible was met were excluded. Amounts are rounded to the nearest dollar or percent.
A substantial portion of silver plans indicated in the Landscape file that their benefit design included a $0 drug deductible. An examination of a subset of the Summary of Benefits and Coverage (SBC) documents from these plans confirmed that two-thirds of the sample of plans actually did not require drugs to be subject to a deductible. The remaining third could not be validated with the data from the plan’s SBC.
View Avalere’s full report attached.
For more information on Exchange plans, contact Caroline Pearson at CPearson@Avalere.com.
Learn More

