Declining WIC Participation May Lead to Poorer Health Outcomes
Summary
With fewer eligible Americans participating in WIC, increased risk of food insecurity and decreased access to quality healthcare may place a greater burden on our healthcare system. The COVID-19 pandemic further exacerbates the challenges of vulnerable populations in access to food resources and routine and acute care.Declining WIC Participation
The Special Supplemental Nutrition Assistance for Women, Infants, and Children (WIC) program provides assistance to low-income women, infants, and children deemed to be at “nutritional risk.” In particular, WIC helps eligible individuals buy certain foods, provides access healthcare, and makes nutrition and breastfeeding education available. WIC is not an entitlement program, so the number of families who may participate is limited by annual Congressional appropriations. States may supplement with their own funding.
After peaking at almost 9.2 million in 2010, the number of participants in the WIC program has fallen steadily each year (see Figure 1). This trend has resulted in a 23% decline in program cost over the last decade. More importantly, it has not just reflected improving economic conditions but also a declining coverage rate (or percentage of those who participate among those who are eligible). While the number of eligible Americans has remained fairly steady, the coverage rate has declined by more than 5 percentage points over the past 15 years. Throughout this period, only about half of eligible Americans have participated in the program.
Even among those who participate, underredemption of program benefits is a common occurrence. In 2012, for example, only 73% of beneficiaries redeemed any of the cash value benefit for fruits and vegetables, which has led the US Department of Agriculture (USDA) to request comments from the public to inform appropriate programmatic modifications.
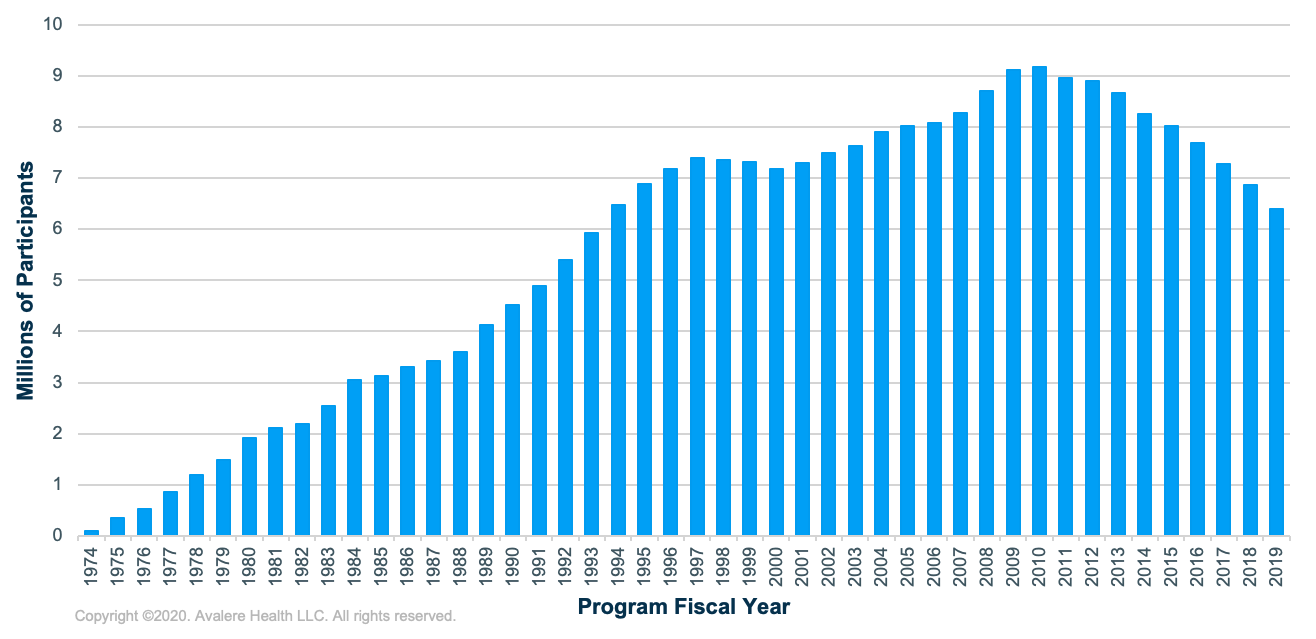
Data source: USDA WIC Data Tables
Notably, this trend is not consistent across states, as 14 states experienced increased participation. Some of this variability may be due to state flexibility in program implementation, such as methods of outreach and registration and the degree of flexibility in their food packages, as well as the degree of success in transitioning to an electronic benefit transfer system. In 2017, coverage rates were below 40% in Montana, New Hampshire, Utah, and Alaska, while they exceeded 60% in California and Maryland. Coverage rates also vary among ethnic groups and have decreased most notably among the Hispanic population over the past decade.
Potential reasons for the decline in WIC participation and coverage include some combination of improving economic conditions, falling birth rates, and concerns about enrollment among immigrant communities, in addition to ongoing barriers related to transportation, stigma, and misconceptions about eligibility. Further, a proposed rule for the Supplemental Nutrition Assistance Program that would have made it harder for states to receive waivers to work or education requirements was set to go into effect on April 1, 2020, and was estimated to put up to 700,000 people at risk of losing benefits. These changes were blocked last month in federal court, however, due largely to the current COVID-19 pandemic and concerns about rising food insecurity.
Studies have typically shown that participants realize a wide variety of benefits (e.g., improved child dietary intake, increased rates of immunization, increased rates of breastfeeding, improved cognitive development) when compared to non-participants. Recent research based on national survey data suggests that since 2010, obesity rates among children participating in WIC have declined while they have increased among all children of the same age range in the US, suggesting a protective effect of access to the food benefits and nutrition education (and possible additional state or local initiatives). However, the downward trend in participation increasingly puts eligible women, infants, and children at higher risk for negative health outcomes
While the COVID-19 pandemic has surely increased the number of Americans eligible for the program, it remains to be seen whether this will translate to increased rates of coverage and benefit redemption. Rising unemployment and job insecurity attributed to the pandemic are contributing to increased food insecurity across the country. Further, while other grocery shoppers may find their choices in grocery stores to be somewhat limited during the pandemic, WIC participants seeking a very specific list of basic staples are having a very hard time finding the food that they can buy with their benefits—especially at the beginning of each month, when benefits are issued.
This has driven the USDA to grant states the ability to apply for temporary waivers to expand their list of approved foods. States may also apply for waivers to roll over benefits between months and eliminate the requirement to come for in-person appointments to issue benefits and recertifications, among other attempts to reduce the burden on program staff and participants. Stimulus funding has enabled the USDA to grant an additional $500 million to states to accommodate the expected increase in participation. But given the inability to conduct in-person appointments and the barriers to access that will continue if not worsen during this public health crisis, these families who continue to be or are newly eligible to participate may not fully utilize their benefits and realize the potential improvements in their health.
Connections to Healthcare
Declining rates of coverage may cause eligible clients to miss out on the information they need to access health insurance through Medicaid, the Children’s Health Insurance Program (CHIP), or other forms of insurance depending on income level and eligibility. WIC counselors (including registered dietitians and lactation consultants) may serve as a front line, offering reminders about necessary immunizations and earlier detection of issues such as stunted growth in children or osteoporosis in women, enabling referrals to specialists for more intensive medical interventions. Otherwise, WIC beneficiaries may not receive needed care. WIC also helps mothers who are unable to breastfeed and children who are malnourished to receive formula and supplements, helping to prevent nutritional deficiencies and malnutrition. More than one-third of WIC clients come from single-parent households, and many do not speak English, which already present structural barriers to receiving quality healthcare. Failing to conduct regular WIC appointments also removes opportunities to recognize issues related to the home environment, such as housing instability or potential domestic abuse, that can be addressed through referrals to other services.
With less access to food resources and education about nutrition and breastfeeding, former participants may experience increased risk of food insecurity and consumption of unhealthy foods. This can result in weight gain and increased risk of chronic disease, ultimately worsening health and increasing the burden on providers and insurance companies to care for vulnerable moms and their children into the future. People in food-insecure households incur roughly 45% higher annual medical costs and are more than twice as likely to skip taking medications as compared to people in food-secure households.
The US is the only developed country in which maternal mortality is rising in recent years, and a huge disparity exists among races and geographic areas. By conducting regular health assessments, supporting behaviors such as breastfeeding and healthy eating, and making referrals to needed social services, the WIC program provides care that can help to stem this rise in crisis that is of concern to policymakers, providers, and insurers alike.
Stakeholders with an interest in maximizing WIC participation, especially during COVID-19, should evaluate the following considerations:
- Continue to optimize the use of telehealth and sharing of health records during the COVID-19 pandemic to ensure adequate screening and monitoring of patients’ conditions and access to needed services.
- Increase program participation by improving screening for WIC referrals among healthcare providers and integrating applications across federal assistance programs to reduce the burden on potential participants.
- Improve coordination between WIC and the healthcare delivery system by improving data-sharing between clinicians’ offices and WIC clinics, enabling the potential health benefits of WIC participation to be reflected throughout patients’ care pathways.
- Further integrate nutrition interventions into healthcare coverage and delivery by better integrating social workers into healthcare settings and conducting more targeted outreach to Medicaid and CHIP patients. Enhancing insurance coverage related to food interventions and nutritional counseling to ensure that patients (in this case, women and their children) have access to nutritious food outside of WIC would also help prevent poor health outcomes and costly treatments.
To receive Avalere updates, connect with us.
January 23, 11 AM ET
Learn More



