Vaccination Rates Among Medicaid Adolescents Declined During Pandemic
Summary
A new claims-based analysis from Avalere examined vaccine uptake among low-income adolescents enrolled in Medicaid Managed Care and found a 26% decline in routine vaccinations when comparing March–October 2019 to the same period in 2020.Policymakers and public health officials may consider a range of policy options to recover vaccination rates among adolescents enrolled in Medicaid Managed Care and to address health disparities that have been exacerbated for low-income populations during the COVID-19 pandemic.
Measures to reduce exposure and transmission of COVID-19, including social distancing protocols, have greatly impacted the delivery of routine healthcare services such as routine vaccination. This has had an impact on the nearly 43 million children and adolescents enrolled in Medicaid, approximately three-quarters of whom live in poverty and many of whom have special healthcare needs. Vaccinations are routinely recommended for this age group and across the life-course to help prevent infectious diseases, certain cancers, outbreaks, and the associated societal and economic costs related to vaccine-preventable diseases. Specifically, the Centers for Diseases Control and Prevention’s (CDC) Advisory Committee on Immunization Practices (ACIP) recommends that adolescents aged 9–18 years be vaccinated against up to 11 infectious diseases.
Multiple studies have shown that routine vaccination decreased during the pandemic. For example, a May 2021 “Morbidity and Mortality Weekly Report” observed a 50% decline in vaccination rates for children across public and private payers in the state of Michigan during 2020. A CDC study further highlighted reductions in vaccine doses ordered through the Vaccines for Children (VFC) program, through which Medicaid-eligible children may receive vaccines free of cost. Additionally, prior Avalere analyses that examined the impact of the pandemic on routine adolescent and adult vaccinations found 13–35% declines in aggregate claims for non-influenza ACIP-recommended vaccines in the commercial, Medicaid Managed Care, Medicare Advantage, and Medicare Fee-for-Service markets.
This analysis found similar trends in vaccine uptake but examines the declines in vaccination services specifically for the adolescent population enrolled in Medicaid Managed Care, which is a substantial population given that over 81% of adolescents and children enrolled in Medicaid are enrolled in any type of managed care plan. This analysis also highlights the back-to-school season from June to October. The findings can help policymakers and healthcare providers advance solutions to recover and improve adolescent vaccination rates for the Medicaid Managed Care population, a historically vulnerable population.
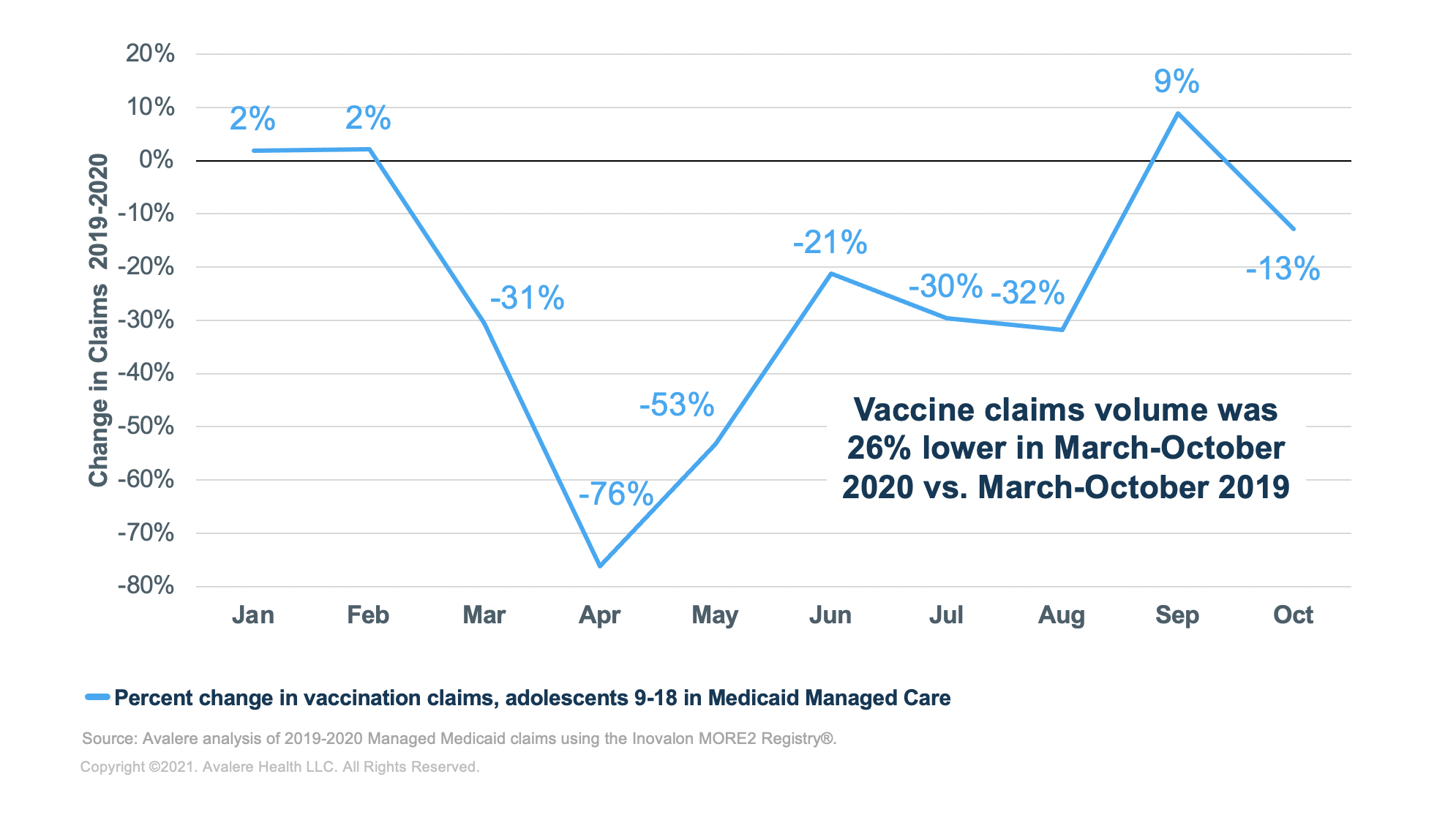
Vaccine Utilization Declined 26% for Adolescents Enrolled in Medicaid Managed Care Plans During the Pandemic
Avalere compared the number of vaccine claims for adolescents ages 9-18 years from January to October 2019 with claims from January to October 2020 for individuals enrolled in a large sample of Medicaid Managed Care plans. Additionally, Avalere analyzed the volume in vaccine claims during the extended back-to-school season (June–October) across both years to understand the impact on this traditionally peak time for adolescent vaccination.
Based on a sample of over 10.6 million vaccine claims in 2019–2020, the analysis found a 26% year-over-year reduction in vaccine claims March–October 2019 to March–October 2020. Vaccination services were down 31% in March 2020 from March 2019, down 76% in April 2020 from April 2019, and down 53% in May 2020 from May 2019. In 2020, vaccine claims volume remained low throughout the back-to-school period, which is typically a common time for vaccination. Throughout the extended back-to-school season of June–October 2020, vaccine claims decreased in volume by 17% relative to the same period in the prior year.
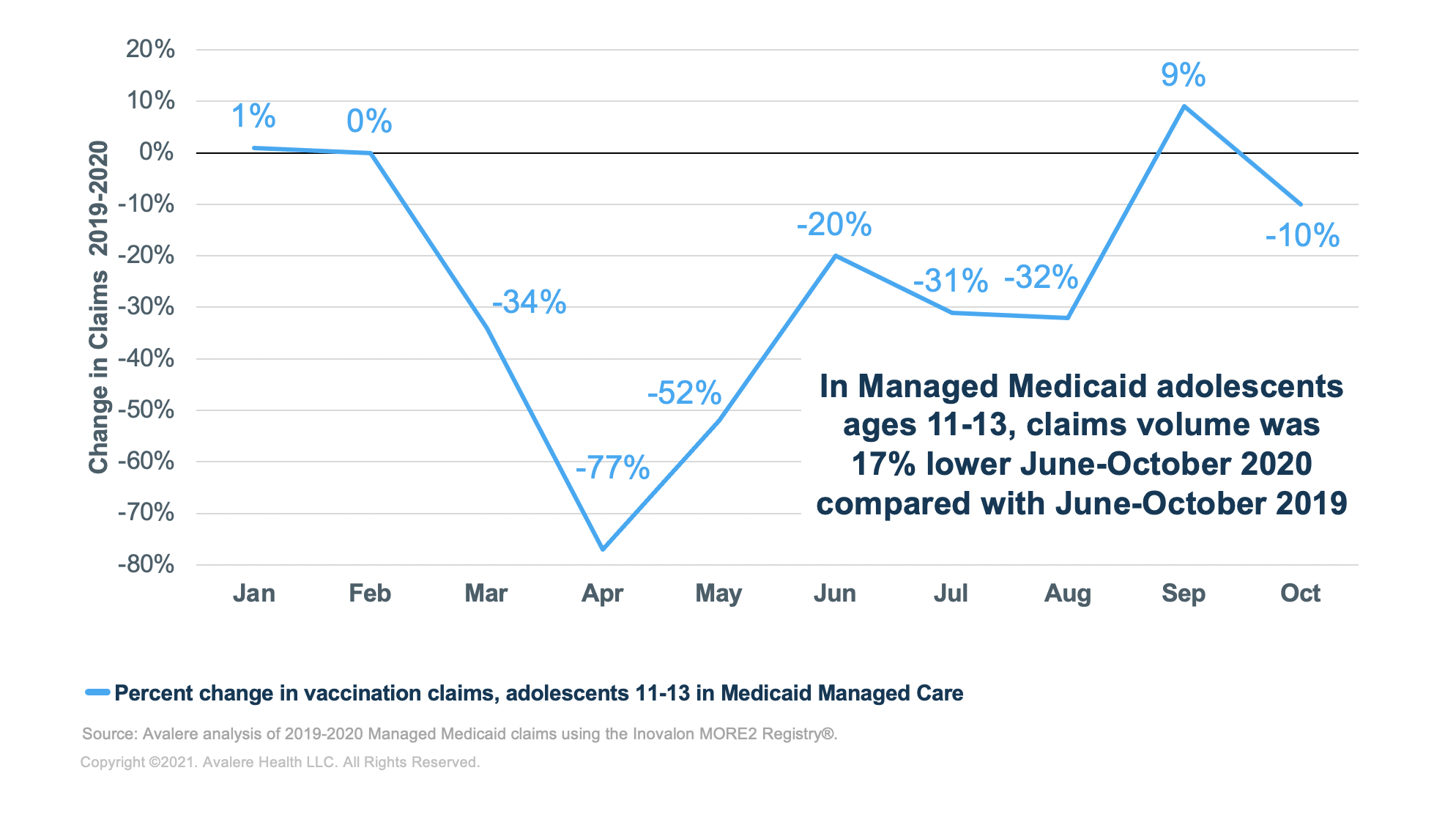
Vaccine Utilization Among the Subset of Adolescents Ages 11–13 in Medicaid Managed Care Also Declined
Avalere also looked at a subset of adolescents ages 11–13 for whom specific vaccines are recommended (e.g., human papillomavirus, Meningococcal and Tdap). This population showed similar declines in vaccination claims when compared to overall adolescent populations. Within this subgroup, vaccinations were down 34% in March 2020 from March 2019, 77% in April 2020 from April 2019, and 52% in May 2020 from May 2019. The volume of vaccines claims for the extended back-to-school period of June–October was 17% lower in 2020 than in 2019 for this subpopulation.
Discussion
While guidance from the CDC has recommended that patients continue to receive routine care during the public health emergency, Avalere’s analysis suggests that the COVID-19 pandemic has reduced the vaccine claims volume and vaccination rate among enrollees in Medicaid Managed Care. These findings are consistent with previous analyses that have demonstrated a significant decline in vaccination rates during the pandemic.
Policymakers and public health officials may consider a variety of strategies to recover vaccination rates among adolescents enrolled in Medicaid Managed Care and address health disparities for low-income populations beyond COVID-19. While each solution will need to be tailored to the population and individual circumstance, some solutions include:
- Focusing on parent and provider awareness and education
- Utilizing reminder-recall strategies
- Engaging with Medicaid Managed Care health plans (e.g., quality improvement programs, provider incentives, beneficiary wellness incentives)
- Ensuring adequate provider reimbursement
- Partnering with trusted messengers such as community organizations (e.g., schools, community health centers) to increase patient awareness and build vaccine confidence
- Establishing health center vaccination campaigns and outreach
In the near term, recovery initiatives may focus on the back-to-school season, which has proven to be an important time for routine adolescent vaccination. Such measures will be critical to ensure that adolescents are vaccinated to comply with state school entry requirements, reduce vaccine-preventable disease outbreaks, and help prevent further exacerbation of existing health disparities.
Funding for this research was provided by Merck. Avalere Health retained full editorial control.
To receive Avalere updates, connect with us.
Methodology
Avalere estimated changes in administration of ACIP-recommended adolescent (9–18 years of age) vaccines using medical claims from the Inovalon MORE2 Registry®, a large scale, real-world multi-payer dataset comprising medical, pharmacy, and lab claims, as well as clinical data on more than 332 million de-identified patients. The dataset contains claims across commercial markets (group, individual, and exchanges), Medicare Advantage, and 69% of the US Medicaid Managed Care population. In 2019, Medicaid included an estimated 19.3 million adolescents (age 6–18), of whom more than 81% were enrolled in a managed care plan. Avalere’s analysis captured more than 5.9 million vaccine claims for 13.1 million adolescent Medicaid Managed Care enrollees in 2019 and 4.7 million claims for 12.4 million enrollees in 2020.
Avalere compared billing for vaccine products and administration codes defined by Healthcare Common Procedure Coding System codes and National Drug Codes (NDCs) from 2019 to 2020 to estimate the potential impact of the COVID-19 pandemic on vaccine administration, represented as a percentage change between years. Specifically, Avalere assessed the differences in vaccine claims for all adolescent Medicaid Managed Care doses—regardless of whether or not the VFC modifier was coded on the claim—between the corresponding months of 2019 and 2020 (e.g., comparing May 2019 with May 2020).
Avalere adjusted the analysis to account for any changes in claim sources within the data by employing a “same-store” analysis that requires the same providers and health plans to have submitted claims in both 2019 and 2020 to ensure that reported vaccine utilization changes are not driven by the addition or subtraction of claim sources over time.
The analysis included the following vaccines: influenza; Haemophilus influenzae type; hepatitis a; hepatitis b; HPV; meningococcal B; meningococcal ; measles, mumps, and rubella; measles, mumps, rubella, and varicella; pneumococcal; tetanus-diphtheria; tetanus, diphtheria, and pertussis; varicella; and inactivated poliovirus. A ‘General’ category is used to capture administration codes that are not specific to any vaccine.
Limitations
Over 81% of adolescents and children enrolled in Medicaid are estimated to be in a managed care plan. Due to variability across states in billing requirements for vaccines provided through the VFC program, this analysis may not fully capture national adolescent vaccine utilization in the Medicaid Managed Care market. While the database is nationally representative, representation by county or state may vary. The proportion of children enrolled in Medicaid Managed Care varies by state, with some states having none enrolled (e.g., CT), some with a portion enrolled (e.g., MA), and others having all of their population enrolled (e.g., TN). This analysis may not be representative of adolescents with other coverage types. Additionally, administrative claims data is used for reimbursement purposes; consequently, claims reporting may not fully capture all vaccine administrations. In cases where product codes or NDC codes were not available, Avalere identified vaccine administration codes. These cases represented 2% of claims included in the analysis. Further, Avalere did not control for the cross-payer population shifts between 2019 and 2020 due to the insurance coverage changes. While the same set of managed Medicaid payers were included in the 2019 and 2020 comparisons, changes in the vaccine utilization may be driven by underlying volume of patients enrolled in a given plan/program, in addition to access and clinical practice patterns.
January 23, 11 AM ET
Learn More


