Remote Monitoring Services Flexibilities Will Change as PHE Ends
Summary
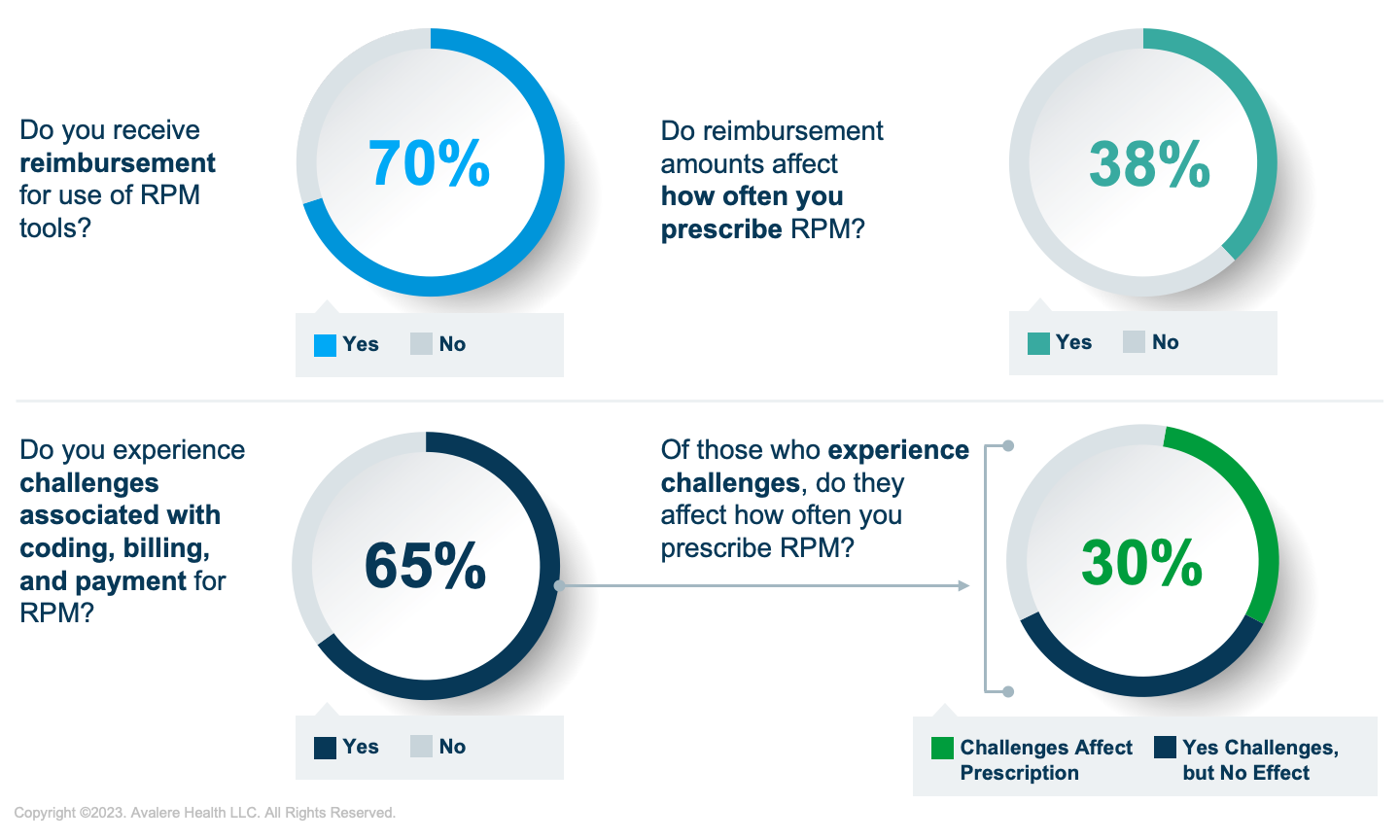
Avalere survey finds 65% of providers experience challenges associated with billing, coding, and reimbursement for RPM.Overview
Remote physiologic monitoring (RPM) is an innovative healthcare offering that leverages technology to provide virtual care to patients at home. As one of many digital health technologies available to patients under the umbrella of remote patient monitoring tools, these systems allow doctors to remotely diagnose and monitor patients, lessening the need for in-person appointments and hospitalizations. The Centers for Medicare and Medicaid Services (CMS) initially labeled RPM as a service furnished to patients with chronic conditions, but clarified in the 2021 Physician Fee Schedule Final Rule that physicians may also provide RPM services to those with acute conditions.
COVID-19 Pandemic Accelerated the Use of RPM Tools
The use of RPM tools has significantly increased during the COVID-19 public health emergency (PHE), given patients’ limited ability to receive in-person care and CMS’s additional telehealth flexibilities. The increased utilization provided new data on RPM’s ability to improve patient outcomes and reduce healthcare costs while providing remote care.
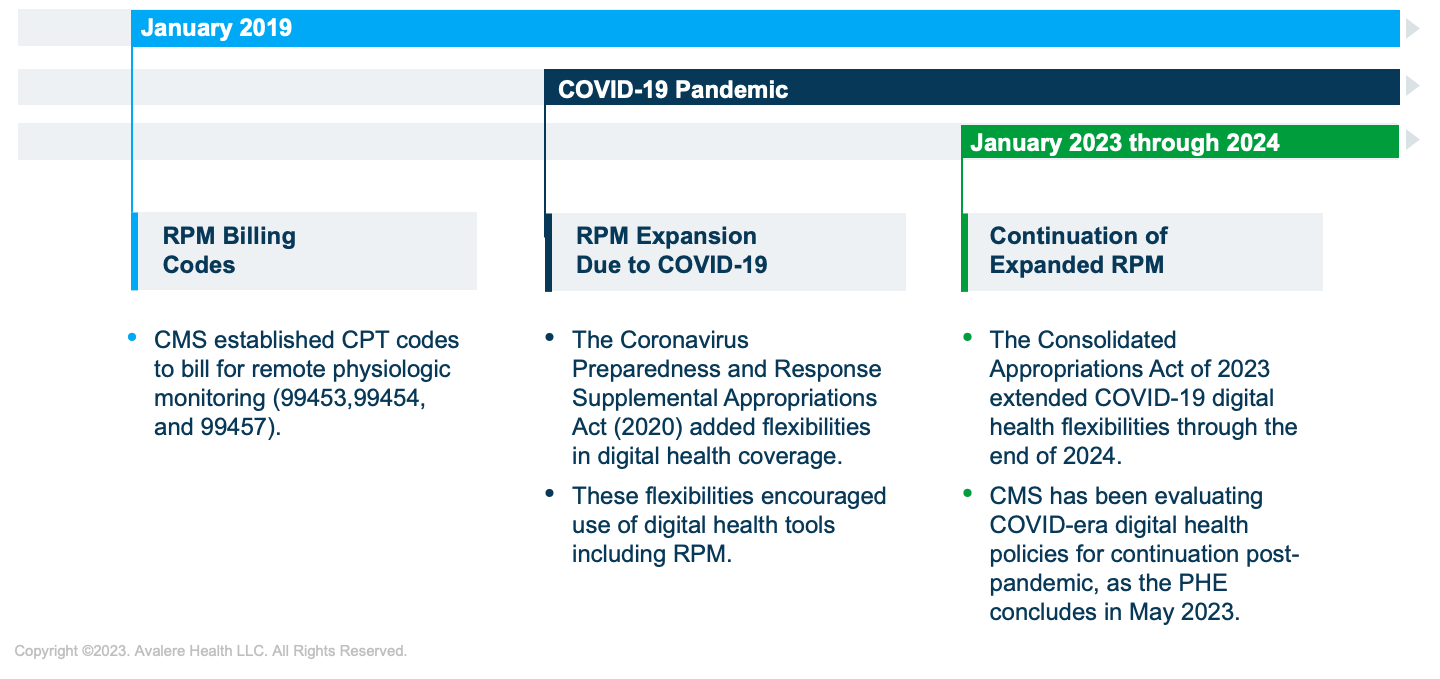
RPM Coding and Coverage Evolved with the Implementation of New Reimbursement Codes
In 2018, CMS implemented new reimbursement codes for RPM services and adopted nuanced guidelines in the Current Procedural Terminology (CPT) codeset. These codes allow healthcare providers to bill for RPM services, including the setup and monitoring of connected devices and the analysis and interpretation of patient data. This reimbursement update has likely led to providers’ increased use of RPM tools with their patients.
While RPM services are reimbursed under Medicare, barriers to uptake still exist. A recent Avalere survey of providers offering RPM services indicated that reimbursement rates and other challenges impact RPM prescription behavior. Barriers include a lack of knowledge of existing codes and various requirements associated with use.
Medicare beneficiaries prescribed RPM services may find that payers may or may not cover the cost of the connected devices used for RPM, meaning that patients could be responsible for purchasing or renting the devices. RPM services and products must meet specific criteria to be eligible for reimbursement under CMS’s established codes. This may include requirements for the RPM devices, patient–provider relationships, and methods of data collection. These requirements may continue to evolve as additional evidence is published.
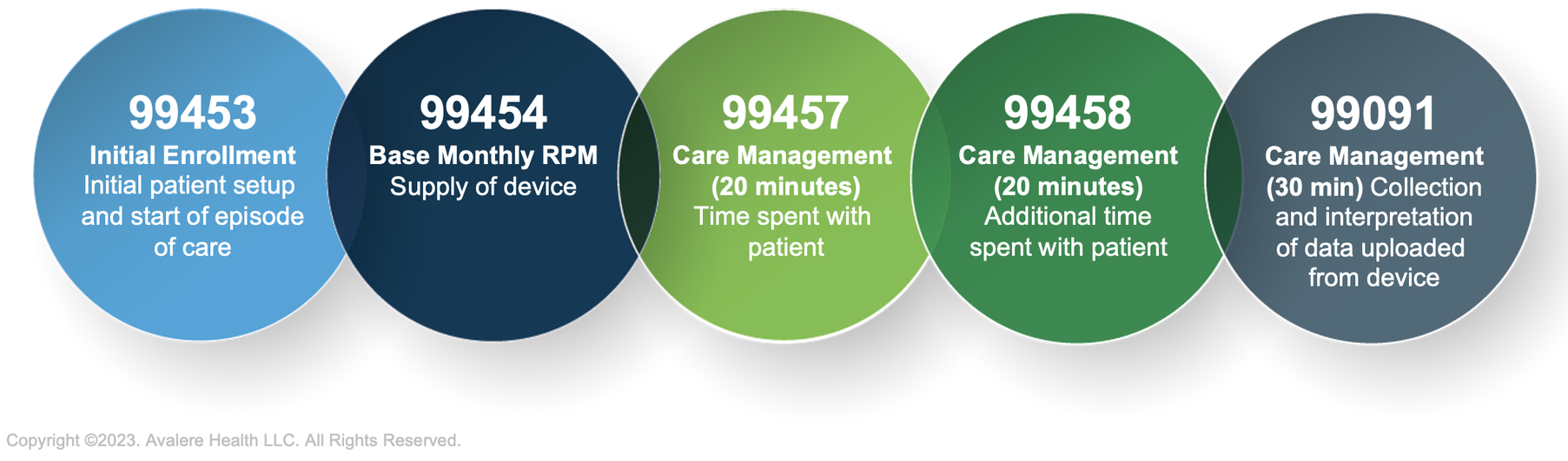
Source: American Medical Association CPT Codes
Recent Coverage Advisory Committee Review Shows Favorable Stakeholder Perspectives for Use of RPM
With the PHE ending in May 2023, stakeholders are actively considering how to maintain uptake and adherence to RPM tools. On February 28, six out of the seven Medicare Administrative Contractors (MACs) met with physician key opinion leaders to discuss remote patient monitoring compared to standard of care and appropriate use cases. Physicians spoke about the opportunities for RPM to reduce hospitalizations and improve patient adherence to treatment. Speakers also highlighted the outcome measures used to track successful RPM use and how RPM can improve equitable access to care. Additionally, stakeholders indicated that coverage decisions by MACs for Medicare reimbursement may indirectly impact RPM across other patient populations. Insights provided during the meeting may provide a foundation for MACs to consider future coverage policy development.
Opportunities for Continued and Increased RPM Use
Stakeholders continue to demonstrate interest in RPM use, recognizing the opportunities and advantages associated with increased utilization. This interest, paired with additional evidence generation, will drive additional discussion around how to improve patient access to RPM, including via changes to coverage and reimbursement. Providers would benefit from increased transparency and communication, as well as a better understanding of specific barriers to RPM uptake across therapeutic areas and patient demographics.
Avalere’s team of experts facilitates dynamic stakeholder conversations regarding RPM and other digital health technologies. To learn more about how we apply our robust expertise at the intersection of digital health technologies and reimbursement, connect with us.
January 23, 11 AM ET
Learn More



