OIG Requests Enhanced Oversight of Remote Patient Monitoring
Summary
The OIG found oversight gaps in Medicare's RPM program, especially in billing accuracy and integrity, highlighting need for safeguards and provider education.Recent Rulemaking Has Defined Parameters for RPM Use
Medicare began covering Remote Patient Monitoring (RPM) in 2018 and has since expanded and clarified RPM covered services and coding best practices through subsequent rulemaking. Medicare has established three main components of RPM: education and setup, device supply, and treatment management; each component has specific associated codes and is paid separately. In the 2024 Medicare Physician Fee Schedule final rule, the Centers for Medicare and Medicaid Services (CMS) established criteria for use of RPM codes in Medicare patients, stipulating that RPM is limited to “established patients,” requires a minimum of 16 days of data collection for device setup and transmission codes (but not for treatment and management codes), and restricts billing to one practitioner per patient within a 30-day period.
RPM Use and Spend Has Increased Significantly
Remote patient monitoring (RPM) has gained significant traction in Medicare, with over 570,000 enrollees utilizing the service in 2022, a tenfold increase since 2019. The Office of the Inspector General (OIG) reports that in 2022, payments for RPM were over 20 times higher than those made in 2019 ($15 million in 2019 and $311 million in 2022). Additionally, the average length of time a patient received RPM and the average RPM payment per patient both increased from 2019 to 2022.
Figure 1: Payments for RPM in Medicare (in Millions)
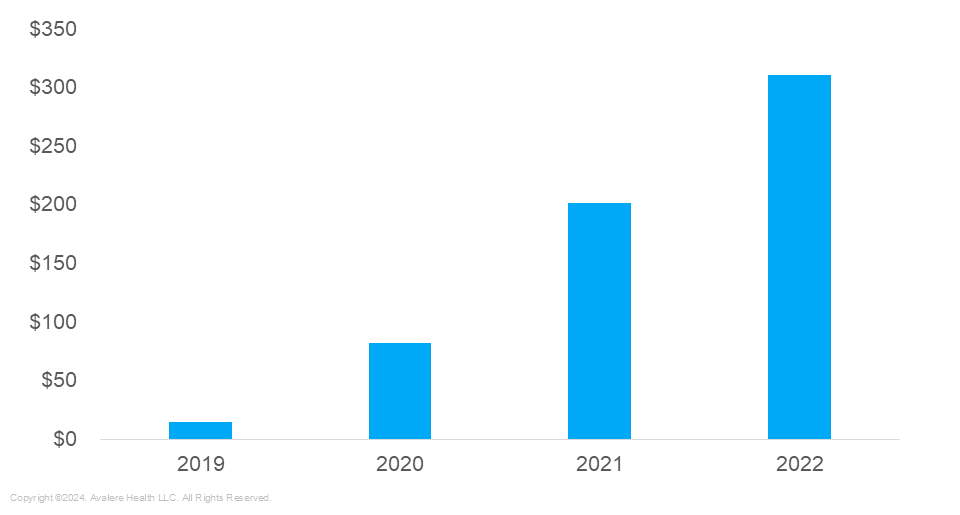
Source: OIG analysis of Medicare claims and Medicare Advantage encounter data, 2024
OIG Report Highlights Potential RPM Vulnerabilities
Despite this growth, a recent report by the OIG highlighted several vulnerabilities in the program’s oversight:
- RPM Usage Growth and Gaps in Implementation: OIG reports that roughly 43% of patients using RPM did not receive the full spectrum of services (i.e., patient education, device supply, and treatment management). RPM is process-oriented, with each component building from the other. CMS does not require providers to bill for all three components of RPM services. However, certain RPM codes should be used in conjunction for comprehensive care and billing. Having such a large percentage of users failing to utilize RPM in its entirety, in conjunction with its components, raises questions about whether RPM is being utilized as intended.
- Fraud and Billing Concerns: Both OIG and CMS have identified significant risks related to fraudulent billing practices, including companies enrolling Medicare beneficiaries in RPM without medical necessity. Often, these companies also fail to provide adequate monitoring services but still charge for them.
- Lack of Sufficient Data Creates Barriers to Understanding Current RPM Use: Medicare lacks adequate data to oversee the specific health data being monitored, the type of devices used, and even the providers who order these services. According to OIG, this lack of data does not sufficiently allow CMS to ensure RPM use meets established requirements.
OIG Recommendations to Mitigate These Issues and Strengthen Value of RPM Use
The OIG report includes three recommendations for CMS.
- Ensure RPM is being billed appropriately:
- Identify providers and/or companies frequently billing for incomplete RPM services and develop data analytics tools to flag suspicious billing patterns.
- Ensure RPM is being used for appropriate diagnosis codes (e.g., conditions that are chronic or acute)
- Mandate that RPM claims include the ordering provider’s details to enhance transparency and fraud detection
- Develop methods to track the specific types of health data being monitored to ensure compliance with Medicare coverage requirements, potentially including the creation of new HCPCS procedural codes or modifiers that allow for health data identification.
- Educate providers nationally, addressing gaps in understanding on adequate and appropriate RPM use and billing.
The release of this report creates opportunities for stakeholders involved in RPM, including manufacturers, digital health developers, and providers, to ensure RPM is being used properly and comprehensively: Refine CMS engagement strategies to ensure that additional safeguards are comprehensive and facilitate continued RPM use, particularly within specialty areas with high RPM uptake (based on 2022 CMS RPM data, the top three specialties were internal medicine, cardiology, and family practice)
- Create an optimized approach for stakeholder understanding of RPM and considerations for compliant use
- Develop training materials and programs to educate healthcare providers on proper RPM use and billing requirements of RPM associated device
- Conduct RPM use-case assessments and scenarios to inform code applicability and appropriate use of RPM devices across medical conditions and patient populations
- Provide additional guidance into any educational materials or provider-facing education that is created by CMS
How Avalere Can Help
Avalere has the expertise to assist stakeholders in navigating coverage, regulatory, and coding challenges, from conducting RPM use-case assessments and scenarios to advising on CMS guidance on RPM. Our team can help ensure that your understanding of RPM services meets Medicare’s evolving standards and position your organization to minimize risks while maximizing patient outcomes. To learn how, connect with us.






