Advancing Diabetes Care in the Era of CGM: Dialogue Proceedings
Summary
As one of the most common chronic conditions in the US—affecting approximately 10.5% of the US population and growing—diabetes (and the optimal management of this condition) remain a persistent healthcare challenge.1In order to document glycemic state and variations, most people with diabetes (PWD) perform self-monitoring of blood glycose (SMBG), which involves pricking the finger to provide blood glucose data at singular moments,2 and complete glycated hemoglobin (HbA1c) testing, which provides data about average glucose control over the past 2–3 months. Even with frequent, routine testing, neither provides complete data about blood glucose trends and fluctuations.3
Continuous glucose monitoring (CGM) uses a wearable device to collect data and provide patients and clinicians with real-time feedback on blood sugar levels.4 Despite potentially providing PWD better data, current use of CGM technology is concentrated among people with Type 1 diabetes (T1D).5 Most people with Type 2 diabetes (T2D), who comprise 95% of all diabetes patients, are managed by primary care physicians (PCPs), who have yet to widely adopt the use of CGM.6
Currently, no CGM-related diabetes quality measures and associated incentives exist, which may inhibit broader adoption. Developing such metrics has the potential to facilitate shared decision-making between patients, improve PWDs’ understanding and management of their diabetes, and offer providers more comprehensive data with which to assess quality of diabetes care. In November 2020, Avalere Health and Beyond Type 1 (BT1) convened a national dialogue meeting, “Advancing Diabetes Care in the Era of CGM,” to consider gaps in diabetes quality of care and identify actionable steps to address them.
The meeting was attended by PCPs, endocrinologists, quality experts, policy experts, and payers, all of whom are active in the diabetes space. Following an overview of ongoing CGM-related activities, Avalere, BT1, and participants discussed the central barriers to CGM use for PWD. A few barriers were identified as the most pressing to address, including low patient and provider education, inadequate provider reimbursement, high patient out-of-pocket costs, and access disparities.
Focusing on the need for quality improvement and evidence generation, participants considered a variety of solutions to address these barriers, including:
- Quality improvement initiatives
- Merit-Based Incentive Payment System (MIPS) improvement activities
- Alternative payment models
These solutions are interrelated, allowing them to be implemented in isolation or sequentially to progress from quality improvement programs and measure development and testing to overall health system transformation. After significant discussion, participants recommended first establishing a quality improvement initiative to set the stage for broader measure adoption and use.
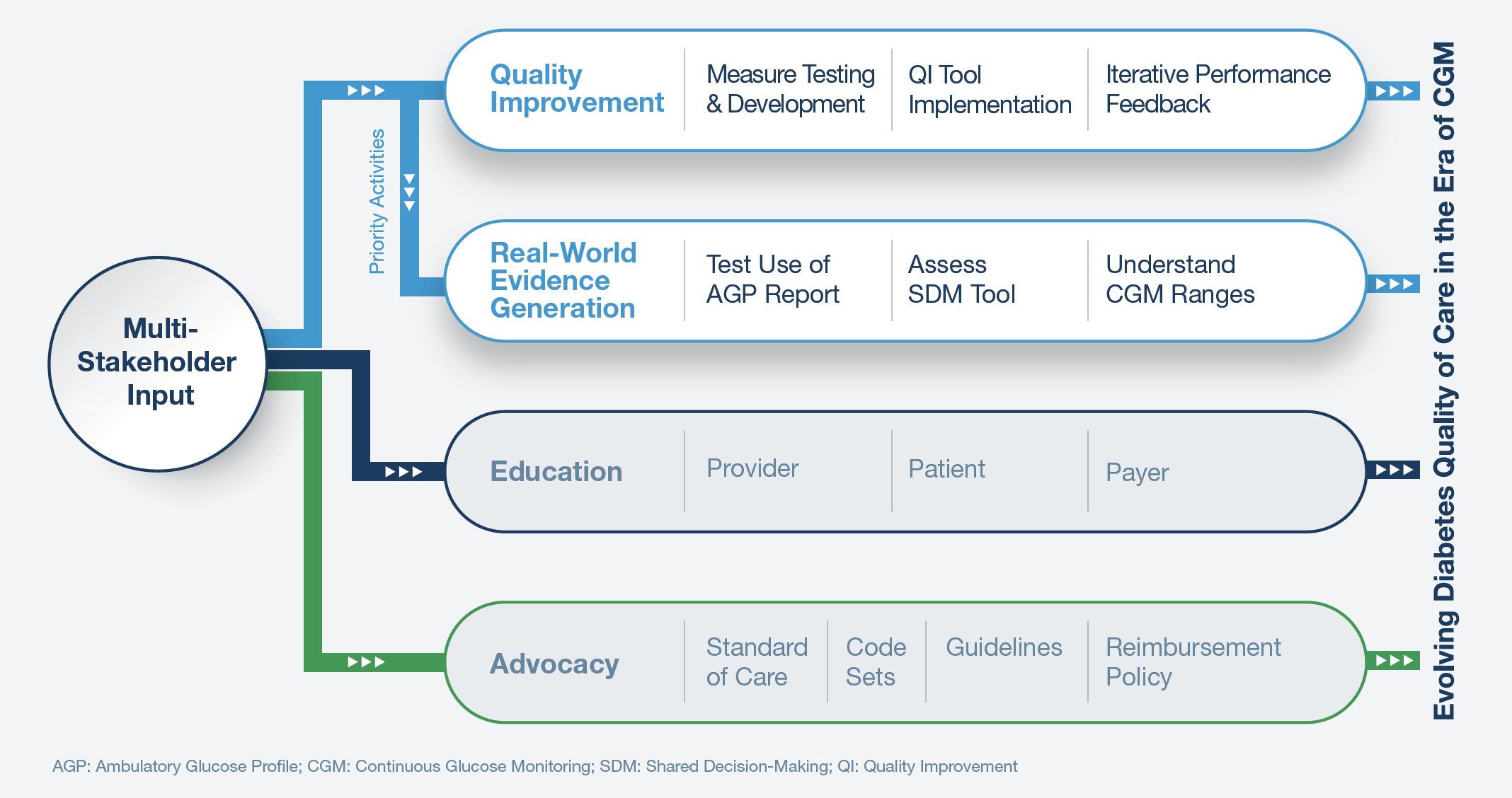
In 2021, diabetes stakeholders will partner to build upon these recommendations by launching the initiative and developing initial CGM-related quality measures. The goal of these and subsequent efforts will be to leverage input from diverse diabetes stakeholders to establish an initiative that advances the quality of diabetes care in the era of CGM (Figure 1).
Download the full proceedings of the Advancing Diabetes Care dialogue sessions.
To receive Avalere updates, connect with us.
Notes
- Centers for Disease Control and Prevention. “National Diabetes Statistics Report, 2020” (accessed April 16, 2021).
- Young, Laura A., et al. “Glucose Self-monitoring in Non–Insulin-Treated Patients with Type 2 Diabetes in Primary Care Settings.” JAMA Internal Medicine 177, no. 7 (July 2017): 920–929.
- Breland, Jessica Y., et al. “Using the Common Sense Model of Self-regulation to Review the Effects of Self-monitoring of Blood Glucose on Glycemic Control for Non-insulin-treated Adults with Type 2 Diabetes.” Diabetes Educator 39, no. 4 (Jul–Aug 2013): 541–559.
- Young, Laura A., et al. “Glucose Self-monitoring in Non–Insulin-Treated Patients with Type 2 Diabetes in Primary Care Settings.” JAMA Internal Medicine 177, no. 7 (July 2017): 920–929.
- American Diabetes Association. “7. Diabetes Technology: Standards of Medical Care in Diabetes—2020.” Diabetes Care 43 no. 1 (January 2020): S77–S88.
- Breland, Jessica Y., et al. “Using the Common Sense Model of Self-regulation to Review the Effects of Self-monitoring of Blood Glucose on Glycemic Control for Non-insulin-treated Adults with Type 2 Diabetes.” Diabetes Educator 39, no. 4 (Jul–Aug 2013): 541–559.






