Air Pollution Connected to Adverse and Inequitable Health Outcomes
Summary
Worse air quality leads to preventable negative health outcomes that increase healthcare costs. Further, urban and minority populations are often exposed to disproportionate pollution risks, leading to impaired health and increased financial burden on both individuals and broader health and social systems.Almost one-third of Americans live in counties with air quality that does not meet national standards. This puts them at increased risk of cardiorespiratory conditions, premature mortality, and reduced quality of life—potentially costing up to $6.4 billion due to excess morbidities and mortalities.
State of Poor Air Quality and Implications for Health
Poor air quality is directly linked to adverse health outcomes. Two pollutants in particular, ground-level ozone and particulate matter (PM2.5) less than 2.5 microns in diameter, are especially harmful to health (see Table 1). High ground-level ozone and PM2.5 levels are linked to the incidence and exacerbation of multiple respiratory conditions, including asthma, bronchitis, upper and lower respiratory symptoms, pneumonia, chronic obstructive pulmonary disease (COPD), and cardiovascular events (e.g., heart attacks). These adverse health outcomes have significant economic implications through increased hospitalizations, emergency department (ED) visits, lost work and school days, and premature death.
Ground-level ozone and PM2.5 are formed through chemical reactions among industrial emissions and between emissions and sunlight, but levels are also significantly tied to warmer temperatures. Alarmingly, air quality and its health effects are worsening; climate change results in increased temperatures and preventable wildfires, and urbanization continues to increase, all of which increase ground-level ozone and PM2.5 levels and the resulting health effects. In 2020, 79.2 million and 50.5 million lived in areas with ground-level ozone and PM2.5 levels worse than the National Ambient Air Quality Standards (NAAQS) set by the Environmental Protection Agency (EPA), respectively. Further, air pollution is not distributed equitably; low-income Black and Hispanic Americans are more likely to live in areas with poor air quality and suffer from the resulting negative health outcomes.
Racial and Ethnic Disparities in Air Pollution Exposure
Although air quality in many parts of the US has dramatically improved since 1980, disparities in exposures and any health benefits experienced by different groups persist. Several racial and ethnic minority groups are disproportionately and systematically affected by air pollution. In 2021, a study published in the American Chemical Society found that 90% of ZIP codes with high levels of PM2.5 were predominantly African Americans. In 2017, another study published in the New England Journal of Medicine showed that African Americans, followed by Asian Americans and Hispanic Americans, face higher mortality risk from long-term PM2.5 exposure.
These groups face greater exposure to air pollution for several reasons. Air pollution is more likely to be emitted and concentrated near low-income communities and people of color. Additionally, there is a correlation between socioeconomic status (SES) and air pollution: populations with low SES have higher exposure to air pollutants and other environmental hazards that can impair their health. Further, people with low SES may have less access to quality healthcare, food, and high-wage job opportunities as well as live in urban areas that tend to be in close proximity to high-traffic areas and the resulting pollutant exposure.
The Biden administration has demonstrated its commitment to environmental health and justice through the Build Back Better Agenda. This plan includes initiatives to decrease pollution and alleviate environmental health burdens through infrastructure improvements and community investments across the US. In March 2021, the American Rescue Plan allocated money for the EPA to direct $50 million toward environmental justice initiatives across the country. Additional environmental measures may pass in the upcoming reconciliation package this fall.
Health Improvements Linked to Addressing Air Pollution
In its 2015 Regulatory Impact Analysis (RIA), the EPA analyzed the potential human health benefits associated with nationally attaining the ozone NAAQS of 70 ppb by 2025 (because a reduction in ground-level ozone corresponds with reduced ambient levels of PM2.5, this enables the EPA to evaluate benefits associated with reductions in both pollutants). The EPA used air quality models and sensitivity modeling runs to estimate the reduction in emissions needed to reach the ozone NAAQS of 70 ppb. It then used various data sources, economic forecasting models, and other statistical methods to quantify the costs to human health and potential benefits that would result from improving air quality. The report showed that improving air quality would result in improved health outcomes, reduced healthcare utilization, and reduced healthcare costs.
A few examples of the burden imposed per ton of pollution over the ozone NAAQS of 70 ppb include:
- 230,000 cases of asthma exacerbation among individuals age 6–18
- 180 respiratory admissions at $37,000 per incident among individuals aged 65+
- 260 nonfatal heart attacks among individuals age 18+
- 80 cardiovascular admissions at $44,000 per incident among individuals aged 18–64
- 160,000 missed school days and 28,000 work loss days
The report concluded that reaching the ozone NAAQS of 70 ppb by 2025 could result in $2.9– $5.9 billion in total potential healthcare savings (overall results summarized in Table 1).
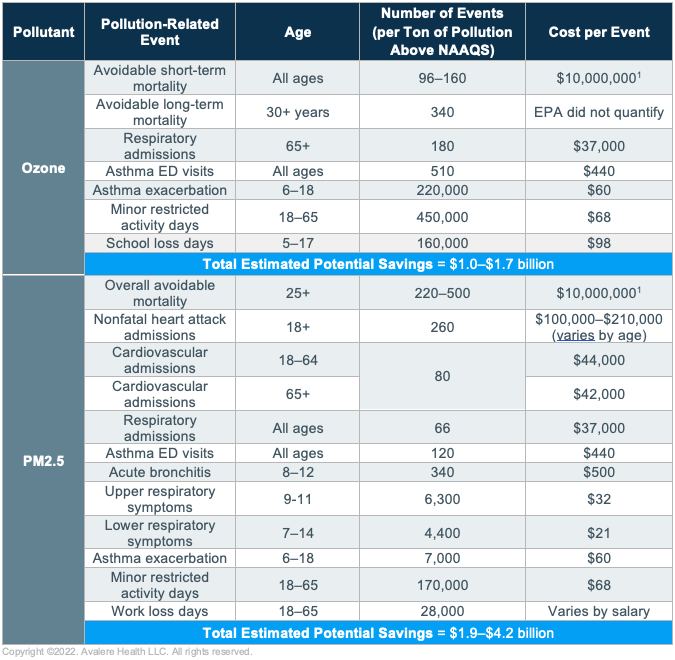
Data sourced from EPA’s Regulatory Impact Analysis of the Final Revisions to the National Ambient Air Quality Standards for Ground-Level Ozone, available here. Parallel analysis for California was conducted separately due to its differing air quality and emissions standards.
1. Reflects the EPA’s Value of a Statistical Life calculation.
Key Considerations and Opportunities for Stakeholders
Considerations for Manufacturers
Manufacturers can engage with environmental health issues by leading translational research to generate real-world evidence related to the effects of air pollution on medication effectiveness, disease management, medication adherence, and healthcare utilization and costs. For example, research could investigate the effects of exposure to ground-level ozone and PM2.5 on the efficacy of an inhaled therapy for COPD or asthma. These studies could also include qualitative data collection to better understand the burden on patients—for immediate health outcomes as well as overall quality of life—and the barriers they face to adherence. Additionally, manufacturers can map air pollution exposure and air quality-associated health conditions, stratified by sociodemographic factors, to identify and target vulnerable patients.
The disproportionate impact of poor air quality is an environmental justice issue and reflects deeper societal inequities in the US. A previous Avalere assessment highlighted ways for manufacturers to engage in health equity initiatives by accounting for the impacts of social determinants of health and health disparities in their market access strategies. Manufacturers can enhance patient engagement programs and develop partnerships with community organizations in areas with poor air quality to facilitate earlier access to screening and educational materials to increase awareness of air pollution risks, associated conditions, and opportunities for improved care.
Manufacturers can also advance environmental health by improving their internal practices. Some manufacturers have developed initiatives that center sustainability across their operations by eliminating fossil fuel emissions, increasing renewable energy use, and reducing the use of hazardous substances. These comprehensive programs set a new standard for life sciences companies to reduce their environmental impact and improve public health.
Considerations for Health Plans
Plans can develop early identification methodologies to monitor pollution risk in their patient population and trigger outreach and intervention when poor air quality is identified. The EPA’s AirNow tool provides up-to-date air quality data by location and could be used to identify at-risk patients. Interventions could include conducting telehealth outreach or deploying case managers to assess patient needs and scheduling a visit with a provider to manage an existing condition. An established protocol to mediate the health effects of increased air pollution would improve patient outcomes, decrease healthcare utilization, and reduce overall cost of care.
Plans can also consider reimbursing in-home services such as home assessments and environmental remediation (e.g., air purifiers or AC units) for patients with asthma and similar conditions. Medicare Advantage plans can provide supplemental benefits for conditions related to air quality and other social determinants of health that affect air quality and respiratory health. Some Medicaid and CHIP programs offer reimbursement pathways for in-home services through Section 1115 waivers; Early, Periodic, Screening, Diagnosis and Treatment (EPSDT) benefits; covered preventative services; and quality improvement activities from MCOs.
Plans can identify providers serving high-risk populations and provide targeted information and training. In a study on Medicaid Managed Care Organizations (MCOs), a program distributing asthma management guidelines to providers in urban areas led to decreased healthcare utilization and a return on investment of $3–4 for every $1 spent by MCOs on program implementation. Another study found a significant decrease in healthcare utilization costs per patient with persistent asthma after a case management team provided educational materials to patients with suboptimal medication use and asthma management guidelines to their providers.
Considerations for Providers
Providers can also establish programs to proactively identify at-risk patients and connect them with necessary resources. Examples of evidence-based tactics may include:
- Establishing home-based education for self-management of cardiorespiratory conditions
- Conducting environmental assessments and home remediation services
- Developing care coordination programs, including referrals to existing social programs
- Ensuring access to community health workers
Larger providers such as hospital systems may be best equipped (possibly through strategic partnerships) to implement comprehensive social programs that mediate the impact of air pollution on human health. One collaboration in Northern Virginia between the state’s primary weatherization provider and a leading healthcare system conducts home improvements for residents whose living situation is leading to or exacerbating health conditions. This effort creates optimal living situations to reduce the harmful effects of air pollution on health. Nonprofit hospitals can also strategically direct their community benefit spending toward these activities.
Avalere has robust expertise in marketplace and regulatory trends, data collection and analytics, and strategy development for these and other types of organizations. Our extensive experience enables us to provide clients with valuable insights to maximize the impact of their programs to further advance health equity and improve patient and public health. To receive Avalere updates, connect with us.
January 23, 11 AM ET
Learn More


