CMMI Program Savings Fall Below CBO’s 2016 Projections
Summary
CMMI’s impact on Medicare spending has so far not reached earlier projections by the Congressional Budget Office, demonstrating the difficulty in projecting savings from new and unknown alternative payment models.In 2010, the Congressional Budget Office (CBO) projected $1.3 billion in net federal government savings from the Center for Medicare & Medicaid Innovation (CMMI) when it scored the budgetary impact of the Affordable Care Act over the 2010–2019 budget window.1 In 2015, the CBO began projecting more substantial savings from the CMMI: $27 billion in net federal government savings over the 2016–2025 budget window, and then in 2016, $34 billion in net federal government savings over the 2017–2026 budget window.2 To explain its higher savings assessment, the CBO noted that although ongoing CMMI demonstrations had not yet generated noticeable savings, it believed that the CMMI would identify successful demonstrations and continue them over the 10-year budget window.
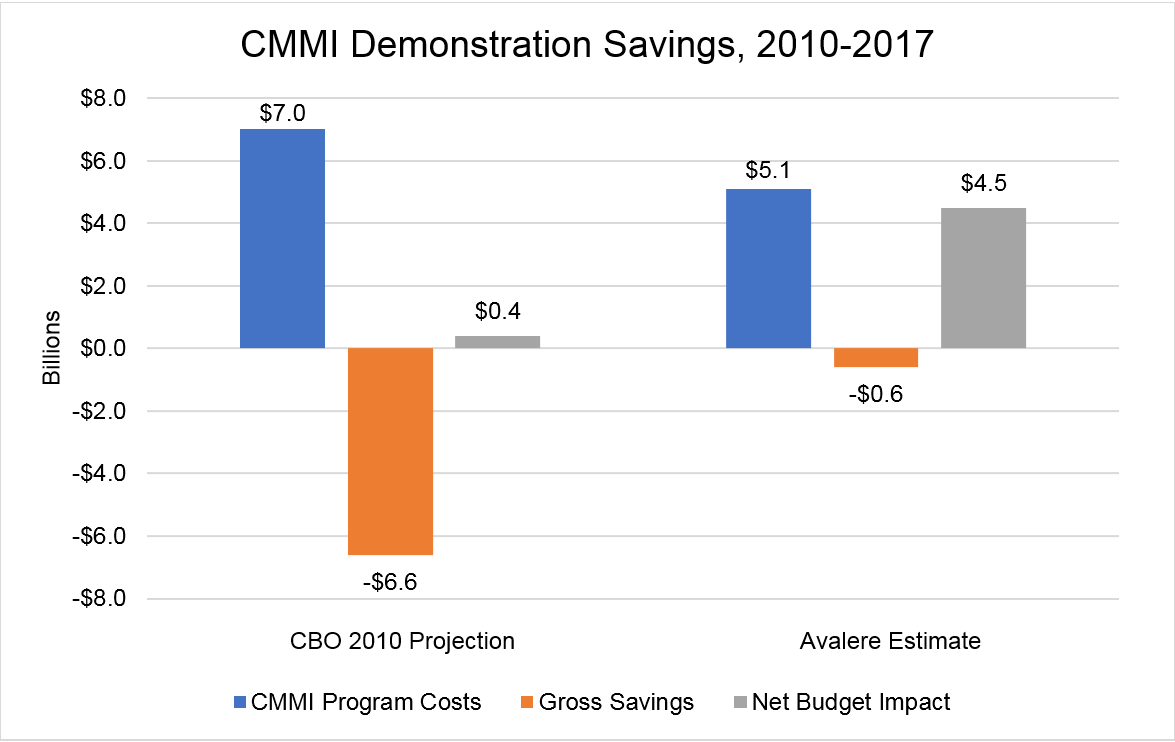
In order to understand how the CBO’s early estimates of expected government savings from the CMMI align relative to experience to date, Avalere examined available evaluations for current or previously implemented CMMI demonstrations. Based on evaluations of CMMI demonstrations, as well as CMMI outlays and funding, Avalere found Medicare savings to be less than the CBO projected—in 2010, the CBO estimated that from 2010 to 2017, the CMMI would increase net Medicare spending by $0.4 billion, while Avalere’s 2019 analysis suggests that CMMI increased net Medicare spending by $4.5 billion during that time period. The CBO projected that gross savings to Medicare (i.e., savings before considering CMMI program spending) would be $6.6 billion from 2010 to 2017, while Avalere found that gross savings were only $0.6 billion. The CBO’s 2010 projections anticipated that the CMMI would initially increase Medicare spending during its early years, with gross Medicare savings from its demonstrations steadily rising over time to achieve greater net Medicare savings. (Figure 1.)
Based on available demonstration results of Medicare net savings achieved from 2010 to 2017 and factoring in expected future demonstration results, Avalere estimates net Medicare savings of $20 billion from CMMI for the 2017–2026 budget window, lower than the $34 billion previously projected by the CBO in 2016 (Figure 2). Avalere’s 2019 estimates include three components, described below.
- Continuation/Expansion of Existing Demonstrations with Reported Savings: The continuation and expansion of already-existing CMMI demonstrations generate $6 billion in gross Medicare savings for 2017–2026. Existing demonstrations that have been found to generate Medicare savings include the Maryland All-Payer Model, Next Generation Accountable Care Organizations (ACOs), Comprehensive ESRD model, Comprehensive Primary Care Plus (CPC+), and Comprehensive Care for Joint Replacement (CJR). When results from evaluation reports are preliminary or only available for the first or second year of the demonstration, Avalere assumed similar performance for later years of the demonstration.
- Implementation of Proposed Demonstrations: Proposed demonstrations generate $21 billion in gross Medicare savings for 2017–2026. Currently proposed demonstrations, which are expected to start in 2020, include the Radiation Oncology model, the End-Stage Renal Disease (ESRD) Treatment Choices model, and the International Pricing Index for Part B drugs. Avalere’s estimates for proposed demonstrations rely on CMS regulatory impact analyses for proposed demonstrations. Avalere assumes each of the proposed demonstrations are continued through the 2017–2026 budget window, and that they continue to achieve Medicare savings similar to their final demonstration year.
- Future Successful Demonstrations: CMMI will launch new, not yet proposed demonstrations that generate $3 billion in gross Medicare savings for 2017–2026. For estimating savings for new and currently unknown future demonstrations, Avalere assumes that CMMI’s ability to launch successful APMs will continue similarly to its history.
Disclaimer: Avalere assumes no change in CMMI’s $10 billion in 10-year funding and resulting program spending for 2017–2026. Avalere’s assumptions for projecting future CMMI activity are generally consistent with the CBO’s, with the notable exception that Avalere’s projected savings for CMMI rely on demonstration-specific savings estimates, based on program evaluation reports for existing demonstrations and CMS regulatory impact analyses for proposed demonstrations.
Funding for this research was provided by the Pharmaceutical Research Manufacturers of America. Avalere retained full editorial control.
To learn more about Avalere research, connect with us.
Methodology
Avalere reviewed publicly available CMS reports and information on prior and existing CMMI demonstrations to capture demonstration impacts and their resulting savings. In order to estimate the implications for projecting future CMMI savings, Avalere combined the most recent evidence of CMMI demonstration savings with CBO’s stated methodology in 2015 and 2016 for estimating future CMMI savings. In some cases, when evaluation report results were preliminary or only available for the first or second year of the demonstration, Avalere assumed similar performance for later years of the demonstration. In addition, Avalere estimated CMMI program costs by using available data on HHS budget outlays for CMMI through 2019 and assuming no changes in CMMI’s decennial $10 billion appropriations.
To estimate the implications for projecting future CMMI savings, Avalere first estimated the savings impact of expanding successful demonstrations, currently in effect, over the budget window. Similar to the CBO, Avalere assumed that CMMI demonstrations would be continued or expanded only if they were generating savings. These programs include ACOs, CPC+, CJR, Comprehensive ESRD Care (CEC), and Maryland All-Payer Model.
Because CMMI continues to test new demonstrations, Avalere also estimated future Medicare savings for demonstrations that are currently proposed. These proposed demonstrations include the Radiation Oncology model, the ESRD Treatment Choices (ETC) model, and the International Pricing Index (IPI) for Part B drugs. For these proposed demonstrations, Avalere relied on CMS’ Medicare savings projections. In addition, Avalere assumed that CMMI would continue to create new demonstrations over the next ten years that have not yet been proposed, which is consistent with CBO scoring assumptions. Avalere projected the savings impact of future unknown demonstrations by assuming that CMMI would continue to create a similar number of successful demonstrations as it has so far.
Notes
To receive Avalere updates, connect with us.