CMS Proposal Would Increase Provider Payment for Vaccine Administration
Summary
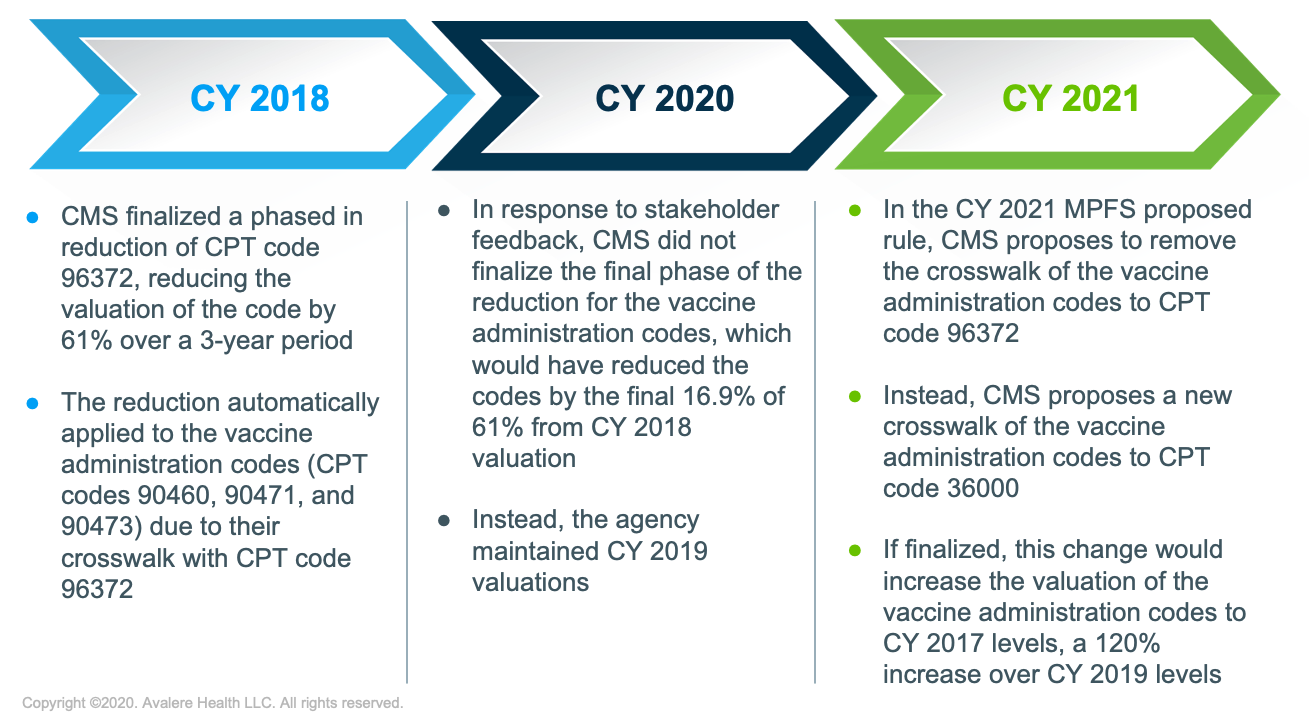
The proposed CY 2020 MPFS rule includes provisions that, if finalized, would increase provider reimbursement for vaccine administration. However, the proposed crosswalk of the codes to a separate, nonvaccine related code could subject the code to future unrelated payment fluctuations.Ensuring adequate provider reimbursement for vaccine administration has been a long-term focus of the immunization stakeholder community. Since 2005, the Current Procedural Terminology (CPT) codes for vaccine administration have been crosswalked to CPT code 96372 (Therapeutic IM or SC administration). In the Calendar Year (CY) 2018 Medicare Physician Fee Schedule (MPFS) rule, the Centers for Medicare & Medicaid Services (CMS) finalized a phased-in payment reduction for CPT 96372, which subsequently would have automatically reduced payments for the vaccine administration codes. The final phase of the value reduction was scheduled to go into effect CY 2020. However, several commenters provided feedback on the CY 2020 MPFS proposed rule that indicated linking the immunization codes to a nonvaccine-related code was inappropriate. In response, the CMS declined to finalize the value reduction for the vaccine administration codes, instead opting to maintain the CY 2019 rates.
In the CY 2021 MPFS proposed rule released on August 3, the CMS included a provision that, if finalized, would adjust the value of the vaccine administration codes by a new crosswalk, specifically to CPT 36000 (Introduction of needle or intracatheter, vein). This proposal would increase Medicare provider reimbursement for vaccine administration by 120%, resulting in payment rates similar to those in CY 2017,1 prior to the finalization of the phased-in value reduction for CPT 96372 (Figure 1). The CMS chose code 36000 because it has similar clinical vignettes and associated practice expenses to vaccine administration; the agency stated it would continue to review the valuations for these codes in the future.
Providers continue to cite the unique level of time and resources required for vaccine inventory management, patient counseling, and claims processing as a barrier to improving low adult vaccination rates. While the CMS’s proposal, if finalized, would effectively increase provider reimbursement for vaccination services, the adjusted value of the code would not be based on actual data on provider expenses associated with vaccinating adult patients. The CMS noted, however, that using the 2009 Relative Value Scale Update Committee inputs would not increase the payment as high as the CPT 36000 crosswalk. This crosswalk does have the potential to subject the immunization codes to future, arbitrary adjustments or fluctuations in value based on the valuation changes of CPT 36000, such as occurred in the CY 2017 MPFS with CPT 96372. The CMS stated that updated practice expense data is needed to revalue the vaccine administration CPT codes and eliminate the need for crosswalking. Such updated data could help ensure that providers are adequately compensated for vaccinations in the future.
To receive Avalere updates, connect with us.
Notes
- The proposal would result in a 120% increase for the primary vaccine administration CPT codes 90460, 90471, 90473. For the add-on on CPT codes 90461, 90472, and 90474, the proposal would result in a 25% increase.
January 23, 11 AM ET
Learn More



