Treatment Disruption due to COVID-19 Poses Challenges to Practices in OCM
Summary
Oncology practices with a substantial proportion of Oncology Care Model (OCM) episodes in areas with high numbers of COVID-19 cases—such as Connecticut, Louisiana, Massachusetts, New Jersey, New York, and Pennsylvania—may face new challenges in containing total expenditure below target amounts.The COVID-19 pandemic has raised new challenges in healthcare management and delivery. These challenges are particularly acute in oncology care, as the reported fatality rate for patients with COVID-19 who had cancer as a co-morbid condition is more than double that of the general population. Not only are patients with cancer at higher risk for contracting COVID-19 and experiencing more severe syptoms but efforts to contain the spread of the virus have also blocked patients’ access to traditional care delivery and support mechanisms (e.g., clinical trial enrollment, 24/7 access to clinicians). As patients and providers implement measures to protect themselves and others from coronavirus (e.g., social distancing, suspension of non-essential services), access and utilization of oncology services will decrease. A recent survey indicated that 27% of patients in active treatment are experiencing cancellation or delays in care (e.g., provider visits, imaging, administration of anti-cancer therapies). More than 13% of patients in active treatment do not know when their care will be rescheduled.
In addition to the clinical challenges associated with treating patients, some oncology practices will face unprecedented financial implications. Practices participating in total cost of care models such as the Oncology Care Model (OCM) are likely to experience changes in expenditure patterns due to care disruption associated with COVID-19. The impact of the pandemic is difficult to forecast as not all patients are able to receive the care they need (i.e., due to limitations in care coordination and patient navigation, delays in initiating therapies, and reduced access to infusion sites), which could lower short-term expenditure. Simultaneously, there are significant costs associated with treating patients with COVID-19, which would increase total expenditures for attributed beneficiaries. In this context, it will be difficult for practices to navigate the model as it is unclear how these variations will manifest in total.
OCM, which recently entered the final year of the 5-year payment program, encourages practices to improve care coordination and contain total expenditure below defined target amounts for 6-month episodes of care. Participating practices are eligible to receive a performance-based payment (PBP) if their costs are below their spending target, and those in 2-sided risk may owe recoupments if their costs exceed a defined threshold. The uncertainty associated with the pandemic will be challenging for practices aiming to maintain expenditure within these defined thresholds.
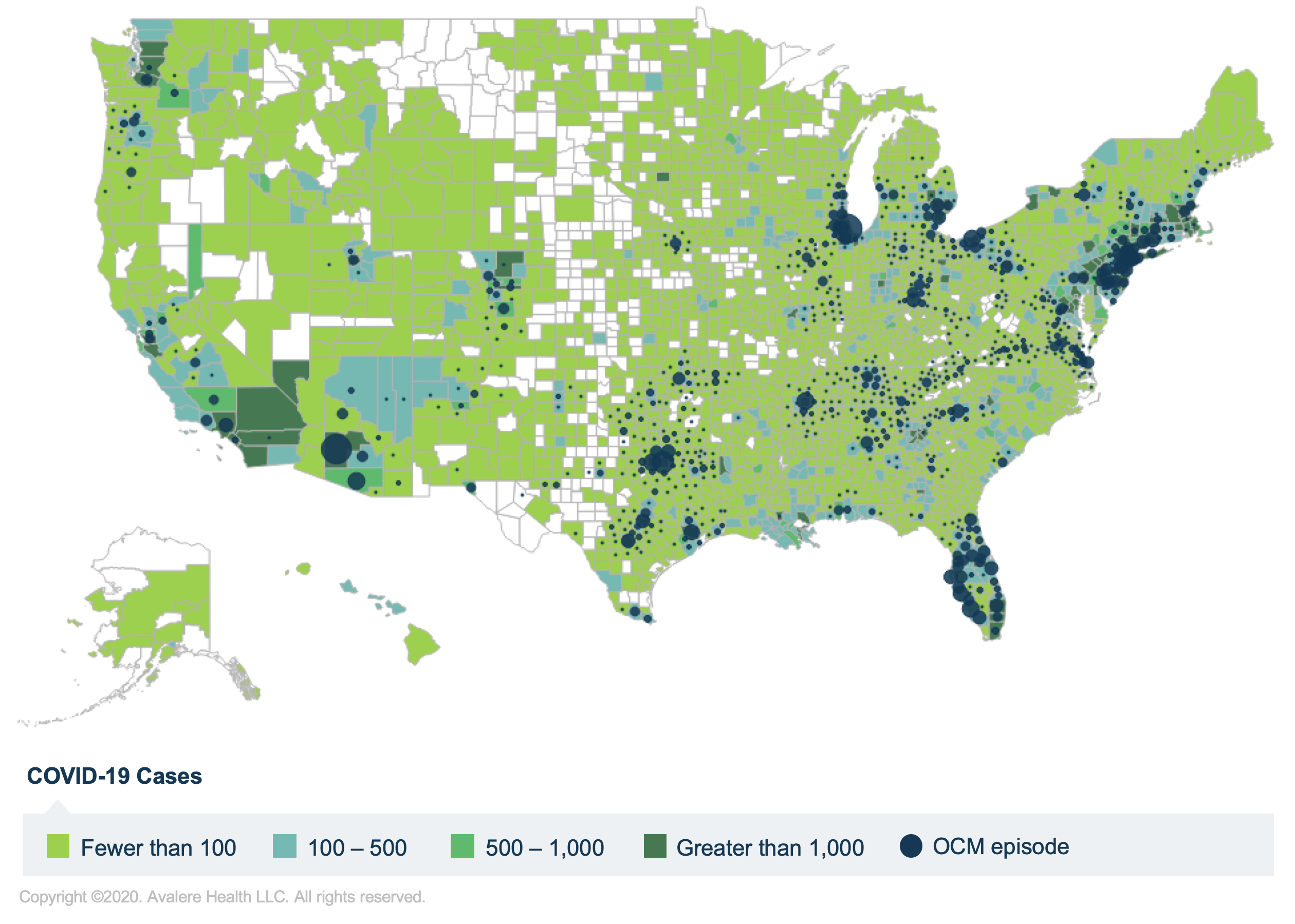
Note: OCM episodes are assigned to the county where the beneficiary resides—beneficiaries may receive care from providers located in different counties. Counties in eastern New Jersey and southern New York have greater than 500 COVID-19 cases.
Avalere analyzed current county-level cases of COVID-19 and prior county-level counts of OCM episodes to understand which geographic episodes might encounter acute disruption of cancer treatment associated with the response to COVID-19 (Figure 1). Practices located in the geographic hotspots of Connecticut, Louisiana, Massachusetts, New Jersey, New York and Pennsylvania will be particularly vulnerable to this disruption (Table 1). For example, while nationally just over a third of all OCM episodes originate in counties with high COVID-19 casess (defined as counties with over 1,000 cases), 71% of OCM episodes in New York would originate from such counties. This suggests that OCM participants in New York are more likely to experience significant changes in expenditures for the current performance period compared to the national average.
Unless the methodology is adjusted, it is unlikely that the prediction model will account for these differences in regional costs, thereby exposing these practices to even greater financial risk. For example, 66% of OCM episodes in Florida originate in counties with low numbers of COVID-19 cases, compared to 7% in New Jersey. Furthermore, the disruption caused by COVID-19 is likely to result in significant downstream implications (e.g., disease progression due to delays in access to care). These downstream effects could impact practices in the next Performance Period and under the proposed Oncology Care First (OCF) model.
| State | Low (Under 500 Cases) | Moderate (500–1,000 cases) | High (Over 1,000 Cases) |
|---|---|---|---|
| Connecticut | 17% | 9% | 75% |
| Florida | 66% | 23% | 11% |
| Illinois | 32% | 7% | 61% |
| Louisiana | 0% | 0% | 100% |
| Massachusetts | 1% | 0% | 99% |
| New Jersey | 7% | 9% | 85% |
| New York | 22% | 7% | 71% |
| Pennsylvania | 30% | 1% | 69% |
| Texas | 48% | 13% | 39% |
| Virginia | 85% | 9% | 6% |
| National | 49% | 13% | 38% |
Estimated costs associated with treating COVID-19 in the intensive care unit (ICU) average $30,950. Avalere compared these projected costs to average per-episode benchmark amounts. In Performance Period 4, the average OCM episode had average expenditures only slightly below the average benchmark threshold, meaning that practices had only a slim margin for cost variation. Adding the estimated cost associated with ICU treatment of COVID-19 to any individual episode would overwhelm the small savings in that episode and would therefore have negative cumulative effects on the participants who were attributed to these episodes. This suggests that practices with high rates of beneficiaries being treated for COVID-19 would be least likely to contain expenditure below their target amounts on aggregate, in addition to experiencing care disruptions associated with the response to COVID-19.
This issue would be particularly difficult for practices enrolled in a 2-sided risk arrangement. In January 2020, practices that had not achieved a PBP in the first 4 performance periods were required to transition to 2-sided risk. A recent survey published by the Community Oncology Alliance found that 37% of participating OCM practices are currently in 2-sided risk. The Center for Medicare & Medicaid Innovation (CMMI) has not yet issued clarity on whether it will offer relief to these practices facing potential recoupment under the model given these unprecedented circumstances. Looking ahead, it will be important to monitor resource utilization as COVID-19 subsides and treatment patterns return to normal in order to inform the CMMI’s decisions regarding performance reconciliation and future structuring of OCF.
Methodology
Avalere performed the analysis of OCM practices using its access to Medicare Part A/B fee-for-service (FFS) claims and Part D prescription drug event data under a CMS research data use agreement. A cohort of patients was selected that includes all OCM-eligible Medicare FFS cancer patients receiving cancer treatment and represented less than 20% of total Medicare beneficiaries. Avalere replicated the OCM payment methodology, including assigning episodes to cancer types, attributing episodes to participating practices, predicting episode costs, calculating risk-adjusted benchmarks, and determining performance relative to the benchmark. Estimated costs associated with treating patients with COVID-19 are derived from a recent analysis published by AHIP. Total confirmed coronavirus cases are based on data from the Johns Hopkins COVID-19 global cases and USA Facts. Please note, there are inherent limitations in COVID-19 case counts associated with testing (e.g., variation in testing methods, false negatives).
To receive Avalere updates, connect with us.
Check out our COVID-19 Intel Center.







