COVID-19 Hospitalizations Projected to Cost up to $17B in US in 2020
Summary
Avalere analysis of Medicare fee-for-service (FFS) hospital stay claims with associated COVID-19 diagnoses finds that total US healthcare system costs for hospitalizations due to COVID-19 could range from $9.6B to $16.9B in 2020.Background
Amid the novel coronavirus pandemic, COVID-19-related hospitalizations have increased significantly, totaling an estimated 293,000 between March and May of 2020. As the number of hospitalizations has risen, costs to the healthcare system for COVID-19 treatment and related procedures have also increased across all health insurance markets, demonstrating opportunity for potential pharmacological treatments and vaccinations to reduce the number and duration of hospitalizations.
Results
Avalere’s analysis of hospital stay claims in Medicare fee-for-service (FFS) found that total costs to the US healthcare system from inpatient hospitalizations due to COVID-19 will range from $9.6B to $16.9B in 2020, depending on 3 scenarios of cumulative hospitalizations through the end of 2020. For comparison, annual hospitalization costs associated with type A and type B influenza have been estimated at $1.3B, with an average of 335,000 hospitalizations per year.1
The largest portion of costs for inpatient COVID-19-related hospitalizations will be paid by commercial payers, ranging from $5.6B to $9.9B. Medicare will bear the second largest portion, paying between $3.5B to $6.2B, including federal government payments for the treatment of the uninsured, as directed by the Families First Coronavirus Response Act (FFCRA), the Paycheck Protection Program and Health Care Enhancement Act (PPPHCEA), and the Coronavirus Aid, Relief, and Economic Security (CARES) Act federal stimulus packages, at Medicare rates.2 Finally, federal and state Medicaid costs are projected to range from $440M to $780M. Avalere’s analysis does not include other provider costs associated with COVID-19, such as staffing pressures, provider supplies and system changes, associated outpatient treatment, and/or other costs outside of hospitalizations.
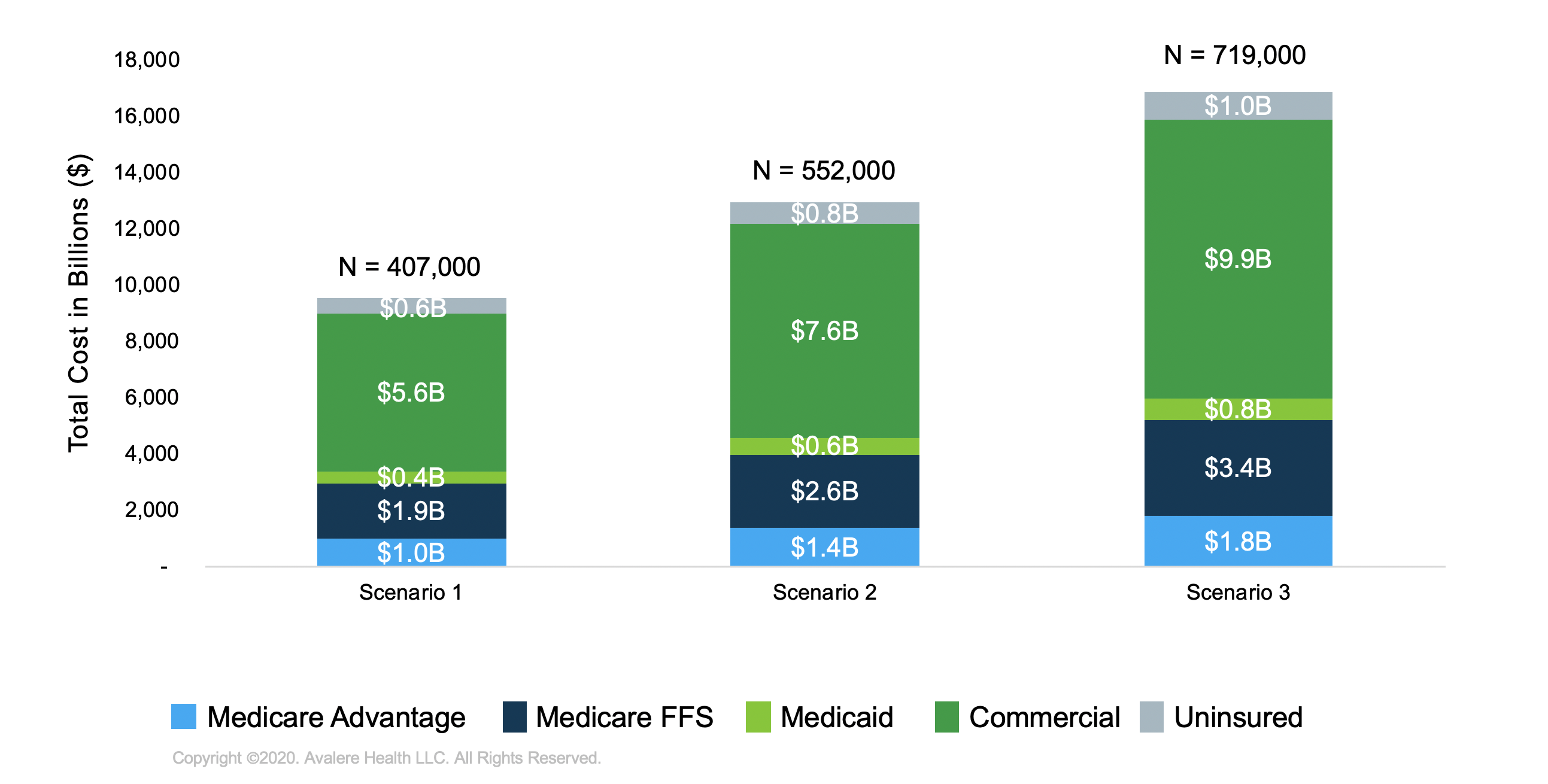
In order to estimate the total healthcare system costs of inpatient hospitalizations to date and through the end of 2020, Avalere developed 3 hospitalization scenarios for 2020 based on the Centers for Disease Control’s (CDC’s) weekly COVID-19-Associated Hospitalization Surveillance Network data from March 7 to June 6. Hospitalizations were then segmented according to likely source of insurance, based on the current hospitalizations by age cohort and race data provided by the CDC.
| Payer Category | Scenario 1 | Scenario 2 | Scenario 3 |
|---|---|---|---|
| Medicare | 185,000 | 251,000 | 327,000 |
| — Medicare FFS | 122,000 | 166,000 | 216,000 |
| — Medicare Advantage (MA) | 63,000 | 85,000 | 111,000 |
| Commercial | 147,000 | 199,000 | 259,700 |
| Medicaid | 39,000 | 53,000 | 69,000 |
| Uninsured | 36,000 | 49,000 | 63,000 |
| Total | 407,000 | 552,000 | 719,000 |
In addition to the scenarios, Avalere calculated the average cost of a COVID-19 hospitalization from February to April 2020 based on Inovalon’s research datasets, which represent 5–7% of all Medicare FFS claims, including charged and paid amounts for hospitalizations. Using calendar year (CY) 2020 pre- and post-adjudicated provider claims, Avalere estimated the average Medicare FFS reimbursement for COVID-19 hospitalizations. This includes key services associated with COVID-19 diagnosis and treatment, such as respiratory ventilation. To account for differences in provider reimbursement across payer categories, the payment rates for Medicaid, MA, and commercial markets were estimated as a percentage of Medicare FFS. For uninsured, Avalere assumed Medicare FFS payment rates.
Avalere then determined weighted average cost per hospitalization by payer to estimate an average hospitalization cost per COVID-19 diagnosed patient of $23,489 across markets.
| Total Cost | Average Cost per Hospitalization | |||
|---|---|---|---|---|
| Payer Category | Scenario 1 | Scenario 2 | Scenario 3 | All Scenarios |
| Medicare | $2.9B | $4.0B | $5.2B | — |
| — Medicare FFS | $1.9B | $2.6B | $3.4B | $15,792* |
| — MA | $1.0B | $1.4B | $1.8B | $16,266 |
| Medicaid | $0.4B | $0.6B | $0.8B | $11,370 |
| Commercial | $5.6B | $7.6B | $9.9B | $38,059 |
| Uninsured | $0.6B | $0.8B | $1.0B | $15,792 |
| Weighted Average | $9.6B | $13B | $16.9B | $23,489 |
* Based on actual April 2020 Medicare FFS claims data for inpatient hospitalizations with a COVID-19 diagnosis.
Variation in Hospitalization Costs
The Medicare FFS data used to estimate the average hospitalization costs captures COVID-related utilization (e.g., length of stay [LOS] and ventilator status) and payment variation across 20 states—those with a sample of 30 or more unique admissions, including California, Michigan, New Jersey, New York, and other initial “hotspot” locations. For this targeted geographic sample, the average Medicare FFS charged amount ranges from $33,000 to $144,000, whereas the average paid amount ranges from $4,700 to $41,000, representing an average charge to payment ratio of 1.30 to 6.42. At the state level, the average Medicare FFS charged amount was $62,216 and average paid amount was $15,792.
The average LOS for admissions requiring ventilation was 13.97 days, nearly 6 days longer than the average LOS (8.04) for hospitalizations that did not require ventilator support. Across all hospitalizations, the average LOS was 9.18. Accordingly, the average Medicare FFS paid amount for hospitalizations requiring ventilation was $31,174, approximately 3 times higher than the average paid amount ($12,140) for non-ventilated hospitalizations.
Conclusion
The results of the analysis indicate that inpatient hospitalizations related to COVID-19 represent significant cost to the healthcare system in 2020, regardless of payer market. As policymakers and stakeholders continue to identify ways to address the spread of COVID-19 in the US, hospitalization cost and provider payment remain a key point of concern, particularly in geographies with high incidence rates. The emergence of potential COVID-19 pharmacological treatment and vaccinations highlight an opportunity to reduce the number of hospitalizations, inpatient length of stay, need for ventilator support, and, subsequently, costs to the healthcare system.
Methodology
Avalere used CY 2020 pre- and post-adjudicated provider claims to estimate the average Medicare FFS reimbursement for COVID-19 hospitalizations. Specifically, Avalere analyzed linked 837 and 835 inpatient Electronic Data Interchange (EDI) transaction sets that were processed during February, March, and April of 2020. The 837 and 835 transaction sets are updated daily and stored in the Inovalon provider research datasets, accounting for approximately 5–7% of the total Medicare FFS volume nationally on average.
As the specific diagnosis code for confirmed COVID-19 cases (U07.1) went into effect on April 1, 2020, Avalere only identified for the analysis hospital stays with discharges that occurred after April 1. After identifying COVID-19 admissions, Avalere estimated the charge-to-payment ratio by dividing each claim’s total charged and paid amounts. The total charges were derived from the outgoing 837 claims, whereas the total payments were derived from the remitted 835 claims. It cannot be determined from the analysis of inpatient EDI transaction sets whether data on paid amounts include the Medicare hospital system add-on payment for COVID-19 patients with an associated U07.1 code during emergency periods, as established by the CARES Act. As a result, reported paid amounts may not account for total provider payment.
Finally, Avalere projected total health system cost for all COVID-19-related hospitalizations in CY 2020. Avalere estimated the total number of COVID-19-related hospitalizations across all payers, including uninsured, hospitalized due to COVID-19 in calendar year 2020 using CDC hospitalization data, both historical and projected weekly hospitalizations. Avalere then developed 3 projection scenarios of weekly hospitalization trends, including a continued decline trend scenario, a slow decline scenario, and a rebound of hospitalizations in fall 2020.
Then, Avalere mapped hospitalizations to payer using the American Community Survey 2018 1-year sample race and age survey data, along with the CDC weekly hospitalization data. Based on the estimated payer mix, Avalere applied a weighted average hospitalization cost (based on what share of people have which form of coverage) and multiplied it by total number of hospitalizations in each of the 3 scenarios to determine the total cost of hospitalization by payer. The inpatient hospitalization payment rates for Medicaid, MA, and commercial markets were estimated as a percentage of Medicare FFS. For uninsured, Avalere assumed Medicare FFS payment rates.
Funding for this research was provided by Gilead Sciences. Avalere retained full editorial control.
To receive Avalere updates, connect with us.
Check out our COVID-19 Intel Center.
Footnotes
- Yan S, Weycker D, Sokolowski S. US healthcare costs attributable to type A and type B influenza. Hum Vaccin Immunother. 2017.
- FFCRA (P.L. 116-127); PPPHCEA (P.L. 116-139); CARES Act (P.L. 116-136).
January 23, 11 AM ET
Learn More



