COVID-19 Impact: Clinical, Social Risk in Skilled Nursing Facilities
Summary
Changes in clinical and social risk among Medicare beneficiaries treated in SNFs at the start of the pandemic reflect challenges facing the healthcare sector during a public health emergency.Avalere analyzed claims for Medicare beneficiaries receiving care in skilled nursing facilities (SNF) at the onset of the COVID-19 pandemic (fiscal year (FY) 2019 – FY 2021) and found that patient acuity and social risk were greater among these beneficiaries than for beneficiaries who received care in SNFs before the pandemic. Although some patient acuity and social risk factors returned to pre-pandemic patterns by FY 2021, the rapid shifts, particularly during the first few months of the pandemic (April–June 2020), highlight the potential for significant changes in the characteristics of patients treated during a public health emergency.
Avalere used Medicare claims data to identify SNF stays and beneficiary demographics and used beneficiary ZIP codes to link to data on characteristics of beneficiary communities (e.g., income, poverty status). Stays with a COVID-19 diagnosis code and stays admitted under the 3-day acute hospital stay waiver were excluded from the analyses to inform changes relative to the population typically treated in SNFs before the pandemic. Avalere examined characteristics of the SNF population during several periods from FY 2019–FY 2021 to track changes in beneficiary characteristics relative to both the start of the COVID-19 pandemic and the introduction of changes to the Centers for Medicare & Medicaid Services’ (CMS) Skilled Nursing Facility Prospective Payment System with the Patient Driven Payment Model (PDPM) in FY 2020.
Key Findings
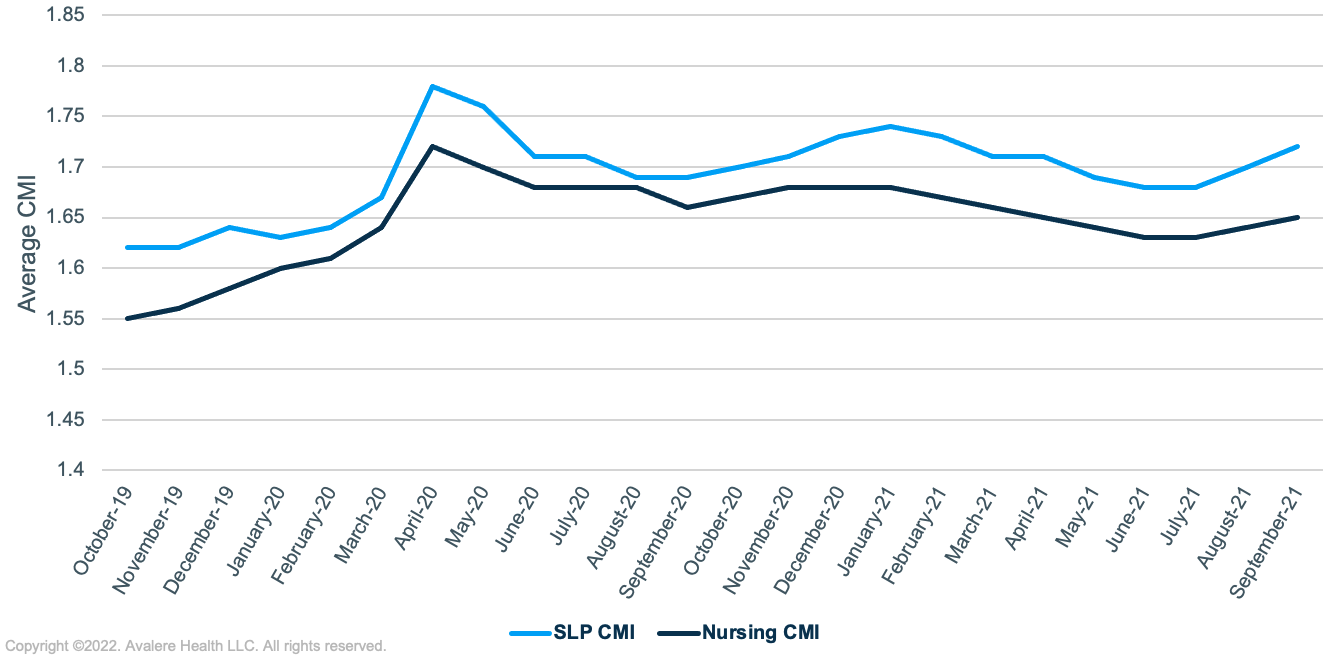
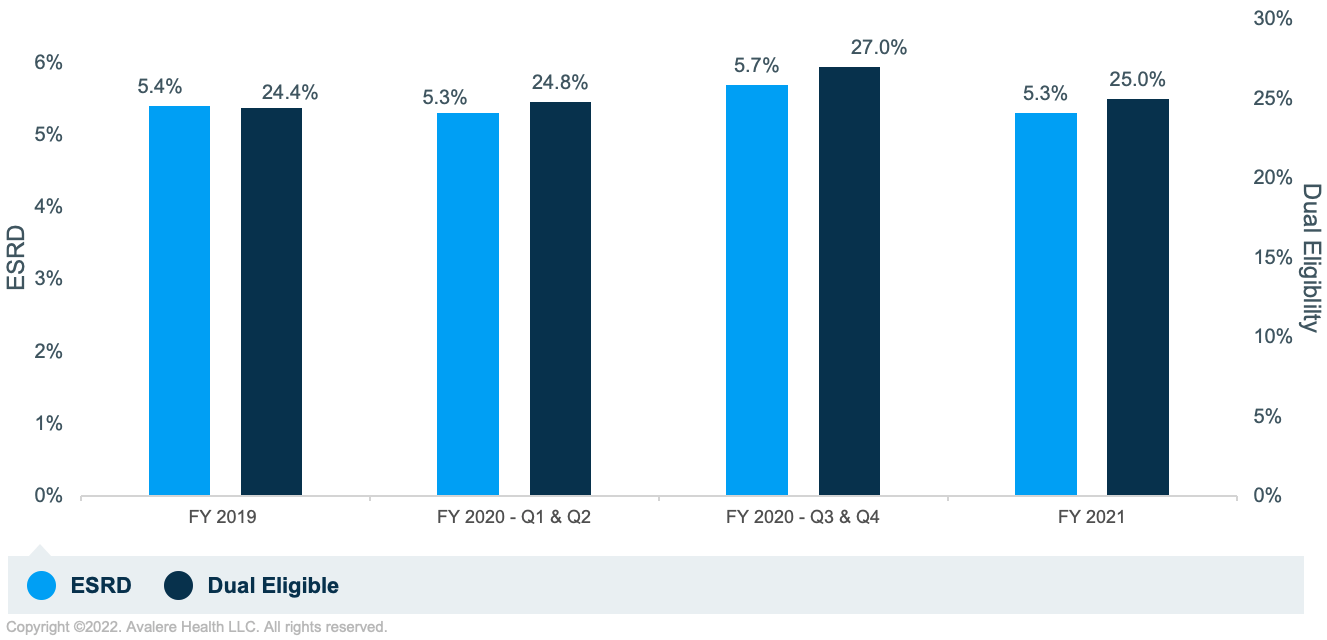
The findings of Avalere’s analyses indicated higher patient acuity among SNF stays at the onset of the COVID-19 pandemic. Medicare beneficiaries receiving care in SNFs had higher case-mix indices (CMI; Figure 1) for nursing as well as for speech-language and pathology (SLP), and a higher proportion of stays were for beneficiaries living with End-Stage Renal Disease (ESRD) and for beneficiaries dually eligible for both Medicare and Medicaid (dual-eligible), indicating higher rates of SNF stays for beneficiaries with high medical complexity and low income status (Figure 2). The average nursing and SLP CMIs remained above pre-pandemic levels into FY 2021. In contrast, the proportion of SNF stays for beneficiaries with ESRD and for dual-eligible beneficiaries returned to pre-pandemic levels in FY 2021.
Avalere also analyzed differences in beneficiary demographics including age, gender, and race/ethnicity in beneficiaries receiving care in SNFs at the start of the COVID-19 pandemic (data not shown) and found small but notable shifts in demographics. For example, the proportion of stays among beneficiaries aged 85 and older decreased slightly between Q1/Q2 and Q3/Q4 of FY 2020 (from 30.5% to 28.7%), while the proportion of stays among male beneficiaries increased slightly during the same time period (from 41.6% to 43.1%). Regarding race, the proportion of SNF stays among Black beneficiaries increased from the first to the second half of FY 2020, from 11.4% to 12.1%.
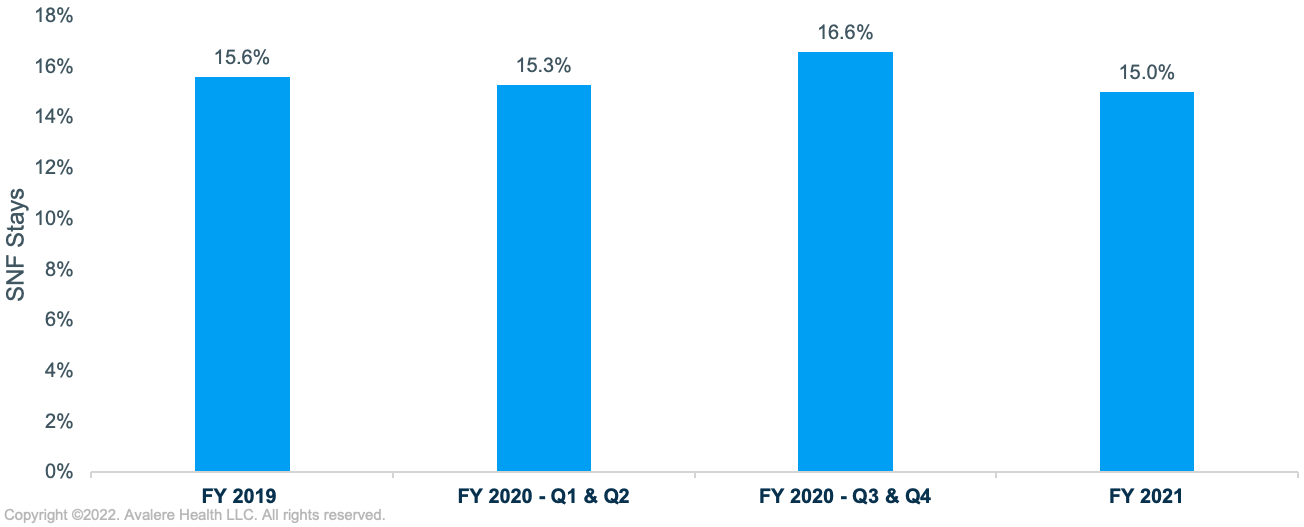
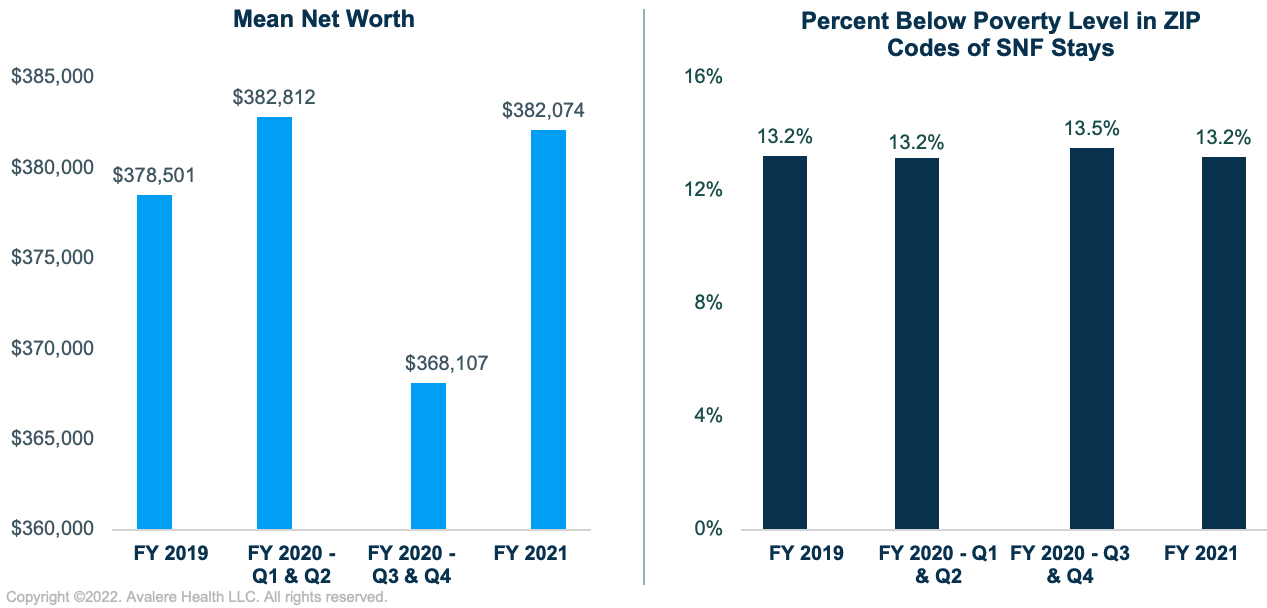
Avalere also identified shifts in the proportion of beneficiaries residing in rural or economically disadvantaged neighborhoods at the start of the COVID-19 pandemic. However, these shifts were minor and returned to pre-pandemic proportions in FY 2021. In the second half of FY 2020, the proportion of SNF stays among beneficiaries living in rural areas increased by 1.3 percentage points (Figure 3). The average net worth in the ZIP codes of Medicare beneficiaries receiving care in SNFs decreased in the second half of FY 2020 before returning to pre-pandemic levels in FY 2021 (Figure 4). Consistent with this finding, the proportion of SNF beneficiaries living in neighborhoods with higher levels of poverty increased slightly in the second half of FY 2020 before returning to pre-pandemic levels in FY 2021 (Figure 4).
Conclusions
Medical complexity and social risk levels increased among Medicare beneficiaries who received care in SNFs toward the beginning of the COVID-19 pandemic. Although the SNF payment system changed significantly with the introduction of the PDPM in FY 2020, observed changes in these clinical and social risk factors were correlated with the timing of the pandemic rather than with the introduction of the payment system. Trends in demographic and socioeconomic factors largely returned to FY 2019 levels after the first wave of the pandemic, although changes in patient acuity, as measured by CMI, persisted into FY 2021. These changes in beneficiary characteristics suggest that the impacts of the pandemic on SNFs was broader than the additional burden of managing patients diagnosed with COVID-19 and understanding changing patient characteristics will be increasingly important as we move to the later stages of the COVID-19 pandemic.
Funding for this research was provided by the American Health Care Association. Avalere retained full editorial control.
To learn more about social determinants of health, connect with us.
Methodology
Avalere used the 100% Medicare fee-for-service claims data to analyze SNF stays from FY 2019 through FY 2021. Claims data were accessed via a research collaboration with Inovalon, Inc. and governed by a research-focused CMS data use agreement.
SNF stays were grouped by admission date (i.e., FY 2019, first half of FY 2020, second half of FY 2020, and FY 2021). The analysis excluded stays with an International Classification of Diseases, 10th Revision diagnosis code of U071 (COVID-19) or with a condition code signifying that the 3-day acute stay waiver (condition code = DR) had been applied.
Avalere used the Medicare claims to identify sex, race/ethnicity, age, disability status, dual eligibility, and rural residence for beneficiaries with SNF stays. Avalere also used Medicare claims to identify trends in the CMIs based on the Health Insurance Prospective Payment System codes. Each of the five CMI components (i.e., nursing, SLP, occupational therapy, physical therapy, and non-therapy ancillaries) is a measure of patient acuity based on diagnoses and patient assessment data and is used to adjust payments.
For socioeconomic characteristics such as mean net worth and percentage of residents below poverty by ZIP code, Avalere linked Medicare claims data to data from Acxiom and the 2019 American Community Survey at the 5-digit ZIP code level.
January 23, 11 AM ET
Learn More
