Emergency State Licensing Flexibilities May Improve Provider Access
Summary
Recent regulatory changes have eased restrictions for providers delivering care across state lines during the COVID-19 public health emergency. However, state and federal cooperation on extended licensure expansion would help address long-term provider access issues.COVID-19 is putting significant pressure on health systems across the country. Providers have shifted focus to COVID-19 treatment, and this shift is impacting provider access for ongoing or acute care needs. Federal and state policymakers have responded by loosening regulatory barriers for providers—including flexibilities to deliver services across state lines either in-person or via telehealth.
As states remain the primary regulators of the healthcare workforce, federal reforms have been limited in effect due to states having more restrictive licensing, supervision, reimbursement, and scope of practice requirements. Increased cooperation between federal, commercial, and state entities around provider licensing and access limitations may help to alleviate COVID-19 related resource burdens. As most of these new licensing regulations last only through the public health emergency, however, states and the federal government may need to work together to consider expanding licensing flexibilities after COVID-19 to ensure long-term access to care. This will be especially important for any future emergencies.
The Federal Government Has Issued Several New Flexibilities for Licensure Under Medicare
Since the federal government declared a COVID-19 public health emergency in March, the Center for Medicare & Medicaid Services has relaxed certain care delivery and reimbursement requirements to allow an expanded provider pool to deliver care to addition patients in additional ways. These provisions include:
- Allowing telehealth to be used for over 80 additional services, by new practitioner types, and at a wider range of service sites
- Approving §1135 waivers to allow licensed Medicare, Medicaid, and CHIP providers to deliver care across state lines
- Allowing expanded staff licensure, certification, or registration in critical access hospitals
However, many of these actions require states to adopt and implement the changes or activate existing state provider regulation flexibilities, creating a patchwork of access and reimbursement obstacles for providers.
State Licensing Flexibilities to Increase Provider Access
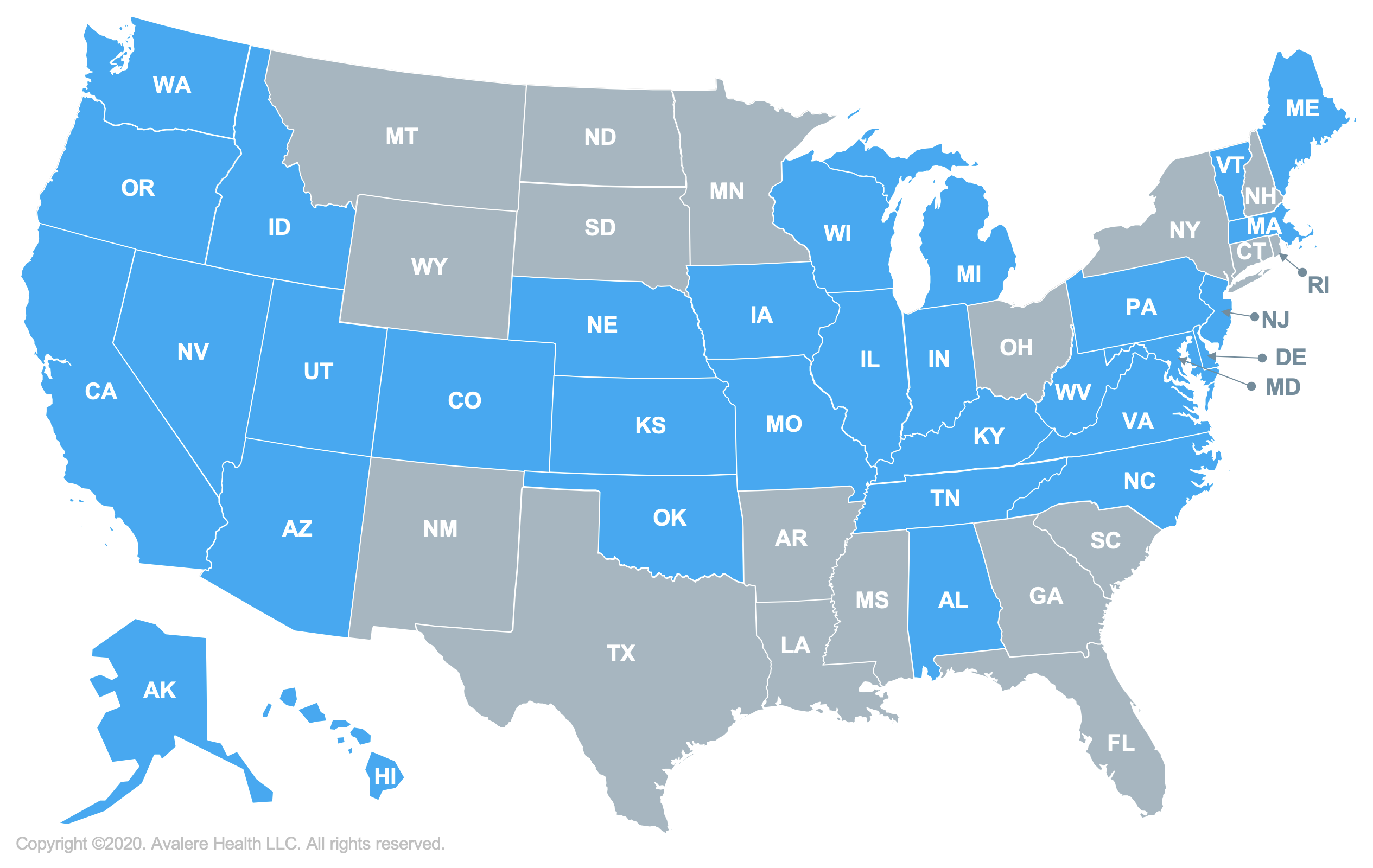
Over the last 2 months, nearly all states (49 states and DC) have issued executive orders, emergency legislation, and orders from state regulatory departments to waive, expedite, or otherwise facilitate new licensing of providers. Many of these actions have targeted new licensing flexibilities that out-of-state providers can use for the duration of the public health emergency. Additionally, more than 30 states are allowing providers who are retired or not currently active to reenter the healthcare workforce through an expedited re-licensing process.
Even with the new actions, not all licensing flexibilities are equally expansive or as quickly effectuated. Some states that have acted still require providers to engage in certain filing or regulatory processes or limit flexibilities to certain providers, in certain settings, and through certain modalities. Providers looking to provide care or seeking additional support for their patients must carefully consider the variations between federal program flexibilities and state provider regulations before engaging.
| Category | Allowing | Not Allowing |
|---|---|---|
| Ability for Providers with Out-of-State Licenses to Practice | 49 States and DC | 1 State (AR) |
| States Temporarily Modifying Telehealth Licensure Requirements | 48 States and DC | 2 States (MI and WA) |
Information on states waiving licensure requirements and state emergency licensure requirements from the Federation of State Medical Boards. Last updated May 5, 2020.
Long-Term Access to Care Through Expanded Licensure Will Require Federal and State Partnerships
COVID-19 has further exposed some of the challenges of provider access shortages in many areas of the country. Not all local facilities and provider pools will be able to meet these needs due to transportation, technology, or resource constraint limitations. State actions relating to licensing restrictions show the varied approaches that may be taken and how federalism concerns can impact the effective long-term implementation of new coverage and reimbursement flexibilities.
As state and federal policymakers craft strategies to address care pathways after the public health emergency, an increased provider landscape may provide greater access to care in states that need it most. Moving forward, states could work with federal program officials and with other states through licensing compacts to provide new flexibilities for provider scope of practice (especially in an emergency) and expand the avenues through which care can be delivered (e.g. across state lines, through telehealth).
Avalere is helping entities to explore the range of ways that these flexibilities could be adopted and implemented, what impact they could have on access to care, what entities need to be engaged, and how to engage policymakers in the process of cooperative design.
To receive Avalere updates, connect with us.







