Fewer Highly Rated MA Plans in 2023 than in 2022
Summary
On October 6, CMS published the 2023 star ratings for Medicare Advantage (MA) plans ahead of the start of open enrollment on October 15.The Star Ratings program measures performance across several domains to provide beneficiaries information to support plan selection. Additionally, star ratings are linked to MA plan payment and quality incentives. MA plans with at least four stars receive higher benchmark and bonus payments that can be used to offer more benefits at no extra cost to beneficiaries.
Each year, the Centers for Medicare & Medicaid Services (CMS) updates the star ratings to incorporate clinical and stakeholder recommendations, new measures, and changes for measure improvement. These updates may affect plans’ ratings. For 2023, CMS altered the methodology for the star ratings, adjusting one measure in response to the COVID-19 public health emergency and the increasing weights for access and patient experience/complaints from two to four.
Highlights from This Year’s Star Ratings Report
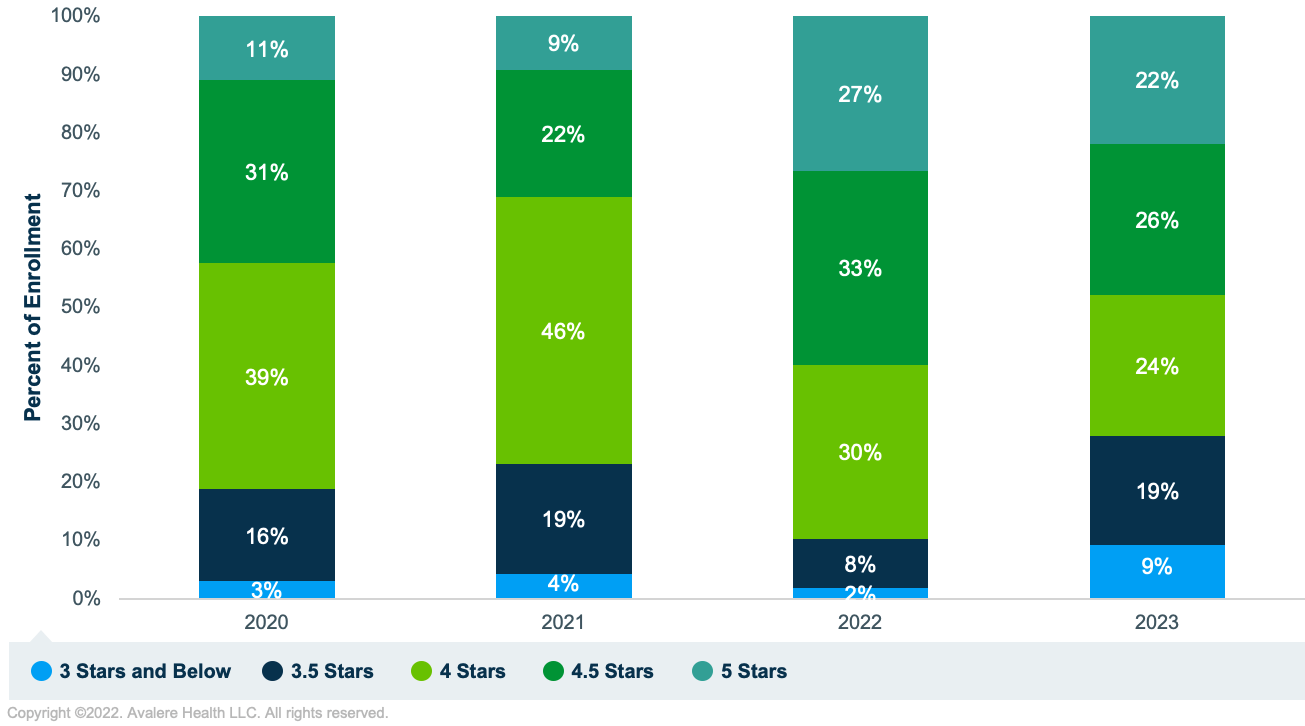
Avalere’s 2023 analysis measures the distribution of enrollees based on their 2022 plan selections. These enrollment percentages could shift in 2023 following the annual open enrollment period that runs from October 15 through December 7.
Fewer enrollees are in Medicare Advantage Part D (MA-PD) contracts with 4 or more stars. For 2022, approximately 90% of enrollees were in MA-PD contracts with four or more stars compared to 72% in 2023, a larger year-over-year shift than in recent years (see Figure 1). In addition, enrollment in 5-star plans decreased by 5 percentage points, enrollment in 4.5-star plans by 7 percentage points, and enrollment in 4-star plans by 6 percentage points compared to 2022. Different parts of the market—e.g., special needs plans that focus on beneficiaries eligible for Medicare and Medicaid—may see different trends than those shown in Figure 1.
*Source: CMS Fact Sheet.
Changes in Star Ratings vary by geography. The average star rating decreased nationally for 2023 to 4.15 from 4.37 in 2022. However, the impact on the number of beneficiaries enrolled in plans with at least four stars varies across metropolitan areas. For example, across the 10 largest metropolitan areas by enrollment, only three areas (Detroit, Dallas, and Houston) had reductions of less than 10 percentage points in the share of enrollees between 2022 and 2023 who are in plans with at least four stars (see Table 1). In New York, nearly three-quarters of enrollees were in a plan with 4 stars in 2022, but only one-third are in a plan with at least 4 stars in 2023.
| Metro Area | Enrollment, September 2022 | Percentage of Enrollees in 4+ Star Plans, 2022 | Percentage of Enrollees in 4+ Star Plans, 2023 | Percentage Point Difference, 2022–2023 |
|---|---|---|---|---|
| New York, NY | 1,242,607 | 74.9% | 33.1% | 42 |
| Los Angeles, CA | 990,902 | 92.5% | 80.7% | 12 |
| Miami, FL | 603,654 | 97.0% | 69.6% | 27 |
| Chicago, IL | 504,624 | 88.7% | 64.1% | 25 |
| Dallas, TX | 461,419 | 86.6% | 83.4% | 3 |
| Atlanta, GA | 432,328 | 83.7% | 60.4% | 23 |
| Houston, TX | 428,156 | 75.9% | 74.4% | 2 |
| Philadelphia, PA | 424,688 | 94.4% | 57.6% | 37 |
| Detroit, MI | 404,230 | 84.3% | 78.5% | 6 |
| Phoenix, AZ | 393,937 | 80.6% | 54.7% | 26 |
**Based on September 2022 enrollment.
As shown in Figure 2, several areas (e.g., Arkansas, portions of Arizona, parts of the Eastern US) had large shifts in enrollment in plans with at least four stars.
Figure 2. Percentage of Enrollees in Plans with 4+ Stars by County, 2022 and 2023
Note: Areas in white have no MA enrollees
Conclusion
The decreases in star ratings likely reflect two main changes: increasing the weights of access and patient experience/complaints measures and the removal of protections, at the measure level, that were in effect in 2022 due to the COVID-19 public health emergency. As a consequence, these lower ratings may impact plan benefits for 2024, because MA-PD plans will use 2023 star ratings in their 2024 bids to determine eligibility for quality bonus payments.
As plans consider how to improve their star ratings in future years, they should focus on a different set of strategies. In past years, plans invested heavily on improving clinical measures outcomes. However, as CMS transitions to more emphasis on enrollee engagement and service, plans need to invest in the development of consumer-centric approaches, including individualized communications and outreach, member-friendly processes and procedures, and real-time evaluation and adjustment of programs. Plans may also want to engage with CMS and measure development organizations to offer recommendations for improvement on measure calculation and evidence generation to ensure that the measures and methodologies accurately capture real-world performance.
To learn more about Star Ratings for MA plans, connect with us.
Methodology
Avalere analyzed 2022 and 2023 star ratings data released by CMS. The analysis reflects MA contracts in the 50 states, DC, and the territories. Avalere excluded Program of All-inclusive Care for the Elderly, Cost, and Demo plans from the analysis. Avalere used plan and county-level enrollment from the September 2022 files. Avalere only included MA contracts with star ratings in both 2022 and 2023 as part of this analysis.




