Health Spending Varies for Patients Likely to Have Obesity
Summary
Among Medicare FFS beneficiaries with diagnoses that are indicative of obesity, total healthcare spending rises dramatically as BMI group increases.Avalere analyzed Medicare fee-for-service (FFS) beneficiaries with diagnoses indicative of obesity to understand how measures of healthcare spending and utilization varied across body mass index (BMI) groups. Diagnoses indicative of obesity are based on direct coding of obesity or a BMI in the obese (BMI of 30+) categories.
Avalere found that per-member-per-month (PMPM) total healthcare spending for patients in the highest BMI group (40+) was 50% higher than that of patients in the 35–39 BMI group, and more than double that of patients in the 30–34 BMI group. This large spending differential among BMI groups was mirrored in the subset of patients with Type II diabetes, hypertension/congestive heart failure (CHF), asthma, and gastroesophageal reflux disease (GERD), conditions that are often associated with obesity. This healthcare spending pattern signals the potential for significant cost savings associated with therapies designed to treat obesity, particularly among patients with certain types of chronic conditions.
Results
Avalere’s analysis shows that total healthcare spending (including outpatient, inpatient, and pharmacy expenditures) rises substantially as BMI group increases (Figure 1). Total healthcare spending increased by $995 (+50%) PMPM for patients in the highest BMI group (40+) compared to patients in the 35–39 BMI group and by $508 (+34%) PMPM for patients in the 35–39 group compared to those in the 30–34 BMI group. The large differential was also observed in patient out-of-pocket (OOP) costs, as patients in the highest BMI group paid $109 (+27%) more PMPM compared to patients in the 35–39 BMI group, and patients in the 35–39 BMI group paid $69 (+19%) more PMPM compared to those in the 30–34 BMI group.
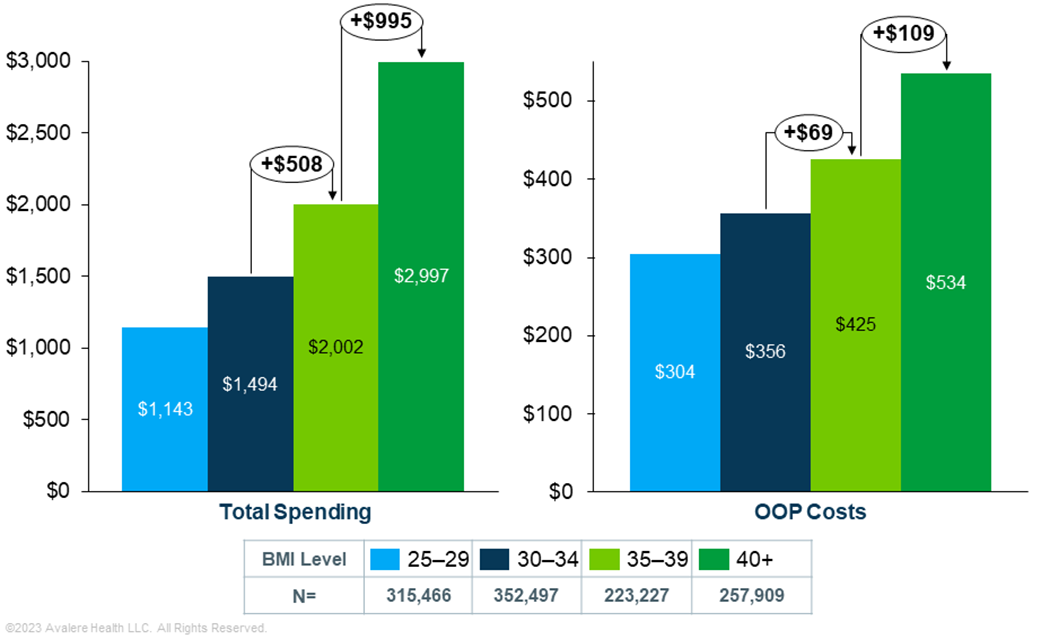
Note: Total spending and OOP costs are shown on different scales to more clearly illustration variations across BMI groups.
Avalere stratified results by five comorbidities commonly associated with obesity: osteoarthritis, Type II diabetes, hypertension/CHF, asthma, and GERD. Patients could be included in more than one group if they had multiple comorbidities of interest. Table 1 shows the prevalence rate of each of the comorbidities within the analysis patient cohort. Across all BMI groups, hypertension/CHF was the most common comorbidity (91% of the cohort), followed by Type II diabetes (43%–64% of the cohort). The prevalence rate of comorbidities rose as BMI increased, except patients with hypertension/CHF.
| BMI Group | Osteoarthritis of the Knee | Type 2 Diabetes | Hypertension/CHF | Asthma | GERD |
|---|---|---|---|---|---|
| N= | 186,591 | 616,428 | 1,0422,695 | 134,085 | 332,238 |
| 25–29 | 11.5% | 43.3% | 90.6% | 7.8% | 27.2% |
| 30–34 | 14.6% | 52.2% | 90.7% | 9.6% | 27.9% |
| 35–39 | 18.0% | 59.0% | 91.1% | 12.4% | 29.2% |
| 40+ | 22.7% | 63.6% | 90.7% | 18.6% | 32.1% |
When assessing total healthcare expenditures by patient comorbidity, the results also demonstrated large incremental increases in PMPM spending as BMI group increased (Figure 2). Total healthcare expenditures were approximately 25–50% higher for patients in the 35–39 BMI group compared to those in the 40+ BMI group for each of the five comorbidities. Patients with hypertension or CHF had the largest incremental total healthcare spending PMPM increases by BMI group (spending increased by 51% for patients in BMI group 35–39 compared to those in the 40+ group), while patients with GERD and asthma experienced the highest total healthcare spending regardless of BMI group.

Discussion
The findings of the analysis show that patients likely to have obesity and be in higher BMI groups experience much higher healthcare expenditures and OOP costs than those in lower BMI groups. The difference in healthcare expenditures incrementally increases with each BMI group, and patients with comorbidities such as hypertension or CHF have even more significant increases in total healthcare spending across BMI groups. These results signal the potential for obesity prevention or treatment to increase patient affordability and significantly reduce healthcare costs and resource utilization. Moreover, treatments that target patients with specific, obesity-related comorbid conditions may yield even larger clinical benefits and increased savings in overall health expenditures.
Life sciences companies launching treatments or therapies for obesity should consider the importance of generating real-world evidence for appropriate target patient populations in support of their value messaging with payers. Additionally, patients with obesity and associated chronic conditions may be particularly vulnerable to social and economic factors (e.g., social stigma, health literacy) that may pose barriers to accessing care. Companies should consider deploying targeted strategies for patient mapping and identification of appropriate support resources.
With a comprehensive approach that includes evidence and strategy, market access, policy, and data analytics, Avalere helps clients understand the evolving landscape for access to obesity care, support research efforts, model the impacts of policy changes, and position for success in the market. Read about Avalere’s recent Insight on anti-obesity medication use and costs.
To learn how Avalere can help your organization respond to—or shape—the evolving obesity landscape, connect with us.
Methodology
This analysis used 100% Medicare FFS and Part D prescription drug event data for calendar year 2019, accessed via a research collaboration with Inovalon and governed by a research-focused Centers for Medicare & Medicaid Services data use agreement. Avalere identified the analysis cohort as patients satisfying at least one of the following three criteria:
- Presence of a primary diagnosis of BMI over 25 in at least one inpatient, hospital outpatient, or physician claim
- Presence of obesity as a primary diagnosis, with BMI as a secondary diagnosis on at least one inpatient, hospital outpatient, or physician claim
- Presence of a target comorbidity (Type II diabetes, hypertension/CHF, asthma, GERD, osteoarthritis of the knee) as a primary diagnosis, with BMI as a secondary diagnosis on at least two claims
The vast majority (97%) of the overall patient cohort met the third criteria related to target comorbidities.
Avalere calculated spending measures on a PMPM basis to standardize comparisons. Measures were calculated by dividing patient-level spending by the number of months from the index diagnosis in 2019 to the end of the year. The index diagnosis indicated the first claim in 2019 that met any of the above criteria.
January 23, 11 AM ET
Learn More


