Impact of the COVID-19 Pandemic on Sickle Cell Disease Management
Summary
Sickle cell disease (SCD) is a severe red blood cell disorder that disproportionately affects African-American and Hispanic populations. In the United States, there are approximately 100,000 individuals living with SCD (although there is a lack of accurate reporting and the exact number is unknown).People with SCD experience a multitude of medical complications, including recurring episodes of pain crisis, acute chest syndrome (ACS), infection, stroke, neurocognitive impairment, and cardiovascular disease. These chronic complications require a wide array of medical services and care coordination. Thus, caring for SCD patients is complex from both a medical and health services perspective. This is further exacerbated by the many disparities that plague this community. Discrimination, stigma, lack of treatment options, lack of qualified providers, and challenges with employment and insurance make living with SCD even more difficult. These gaps in care have only intensified in the time of COVID-19. The pandemic highlights the inequities that persist in the treatment of SCD and the impact they have on patients and their families.
Emerging data demonstrate that the COVID-19 outbreak disproportionately affects communities of color. For patients with SCD, these racial disparities take a toll on the community and are further compounded by their disease. SCD experts in practice have shared what care delivery looks like in this current environment.
Common Trends as They Relate to SCD and COVID-19 Treatment
Fear of Seeking Treatment
Clinicians have noticed an overall reduction in the number of SCD patients that seek care, either for their normal visits or for emergent needs. SCD patients and their caregivers understand the vulnerabilities associated with exposing patients to the virus and are erring on the side of caution by skipping appointments or avoiding clinical settings. Physicians suspect that patients who are suffering from great pain while in crises will forgo seeking treatment or relief.
Mischaracterizations of Sickle Cell Complications
SCD patients need to be monitored carefully for complications. A common complication patients face is ACS, which is characterized by chest pain, cough, fever, hypoxia (low oxygen level), and lung infiltrates. Given that patients with a diagnosis of COVID-19 also experience some of these symptoms, there is concern that hospitals are prioritizing the triage for possible COVID-19 in lieu following standard treatment protocols. Therefore, the question is raised whether hospitals are prepared to manage SCD patients who become COVID-19 patients as well.
Inconsistent Telehealth Capabilities
Telehealth has been greatly praised as a potent alternative to in-person hospital and outpatient visits. However, it is not necessarily available to all providers and patients. Some SCD clinicians explained that telehealth quickly became an available resource within other specialty clinics like oncology in response to the COVID-19 crisis. However, telehealth was slow in becoming available for SCD clinics. They explained that prior to the COVID-19 crisis, the adult SCD clinic was already overlooked, underfunded, and understaffed. Now, in light of the global pandemic, setting up telemedicine for an already ignored clinic has been slow to be implemented. Across the US, telehealth has been an underutilized tool to treat and manage SCD. Some hypothesize this is due to factors such as lack of hematologists or trained specialists to administer care to SCD patients or existing poor communications or quality interactions between patients and providers. Studies have found that SCD patients in the US are at particular disadvantage regarding communication with healthcare providers even when compared to a national sample of African-Americans.
Inability to Access Healthcare System
Some already-stressed centers have told patients to stay clear of emergency rooms, urgent care, and clinics, and to instead treat pain at home with oral medications or antibiotics. They are forced to deviate from standard-of-care procedures, which puts patients at risk and sets them up to fail without adequate access to care at home.
Case Study
An anonymized case study crystalizes these issues. On April 1, a 36-year-old living with SCD experienced a pain crisis caused by a leg ulcer infection. He reported chest pain and had a fever. The patient has a history of ACS and sepsis. Historically, his family would have called an ambulance or gone to an emergency department. During the COVID-19 outbreak, out of an abundance of caution, his SCD treatment team instructed him to stay home and treat the crisis with oral pain medications, at-home oxygen, and antibiotics since his hospital is currently a site for COVID-19 screening resulting in numerous cases being treated at that location.
While the pandemic has posed great strains on the global health system, opportunities to reduce gaps of care for sickle cell patients might emerge. Three activities providers have observed in sickle cell management due to the pandemic include:
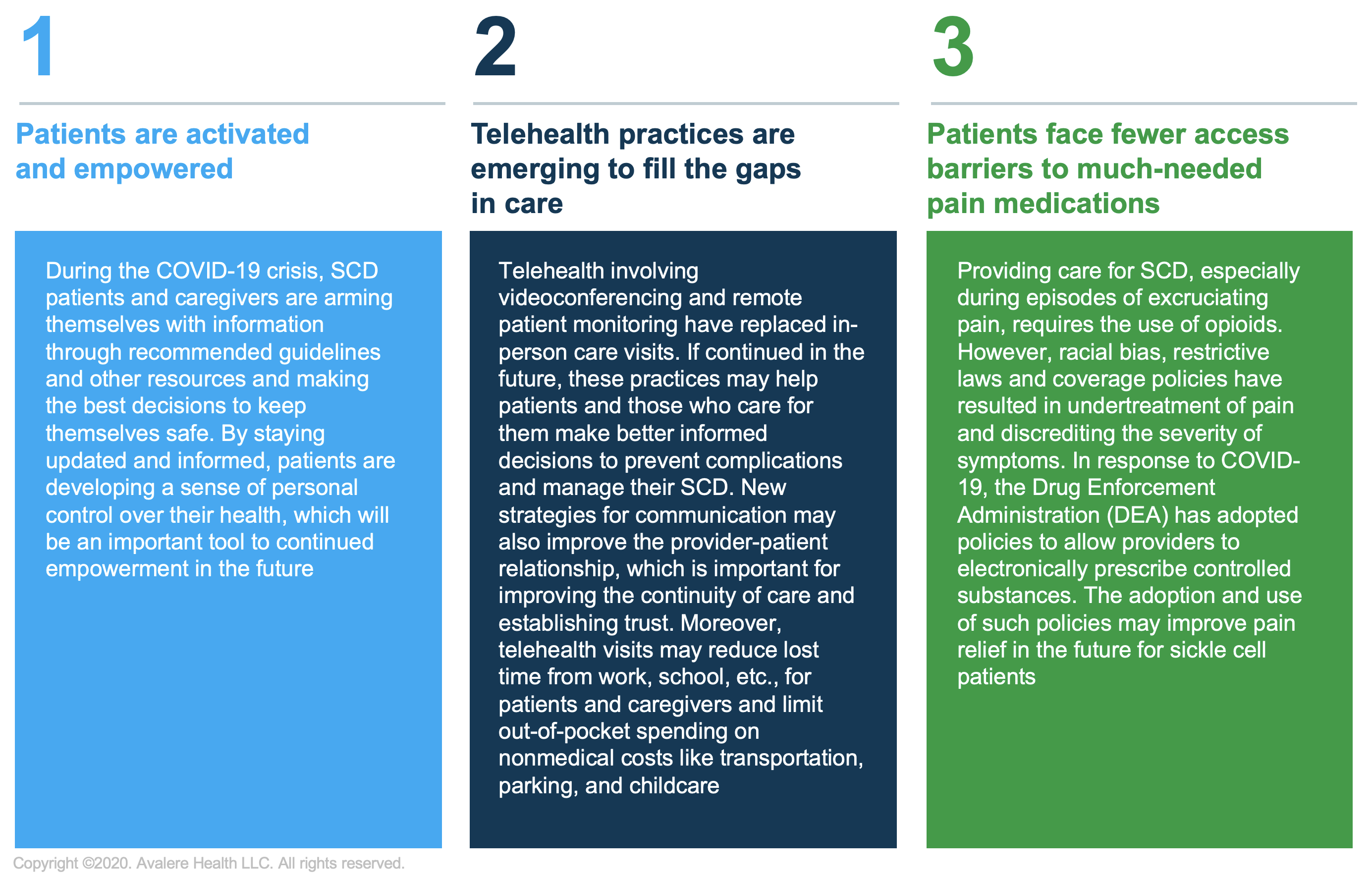
During this challenging time, it is important for both the medical and patient communities to stay united and informed by following clinical guideline recommendations provided by organizations like the American Society of Hematology and the Sickle Cell Disease Association of America. For the patient community, this has been an opportunity to explore new relationships with their providers and healthcare teams while also having the global pandemic shine a spotlight on existing health disparities that have weighed down the community.
To receive Avalere updates, connect with us.
Check out our COVID-19 Intel Center.
This article was co-authored by Avalere and Ashley Valentine and Maggie Jalowsky of Sick Cells. Sick Cells’ mission is to elevate the voices of the SCD community and their stories of resilience.






