RWE Strategy Leads to Support for Avalere-Developed Composite Measure
Summary
Avalere was pleased to partner with the nutrition community to develop and test the Global Malnutrition Composite Score, which has now received conditional support from the Measure Applications Partnership (MAP)—pending endorsement by the National Quality Forum (NQF)—for inclusion in the Hospital Inpatient Quality Reporting (IQR) Program.The measure, developed by Avalere and stewarded by the Academy of Nutrition and Dietetics (the Academy), is the first-ever electronically specified composite measure. It supports a comprehensive approach to address malnutrition identification and treatment in hospitalized older adults.
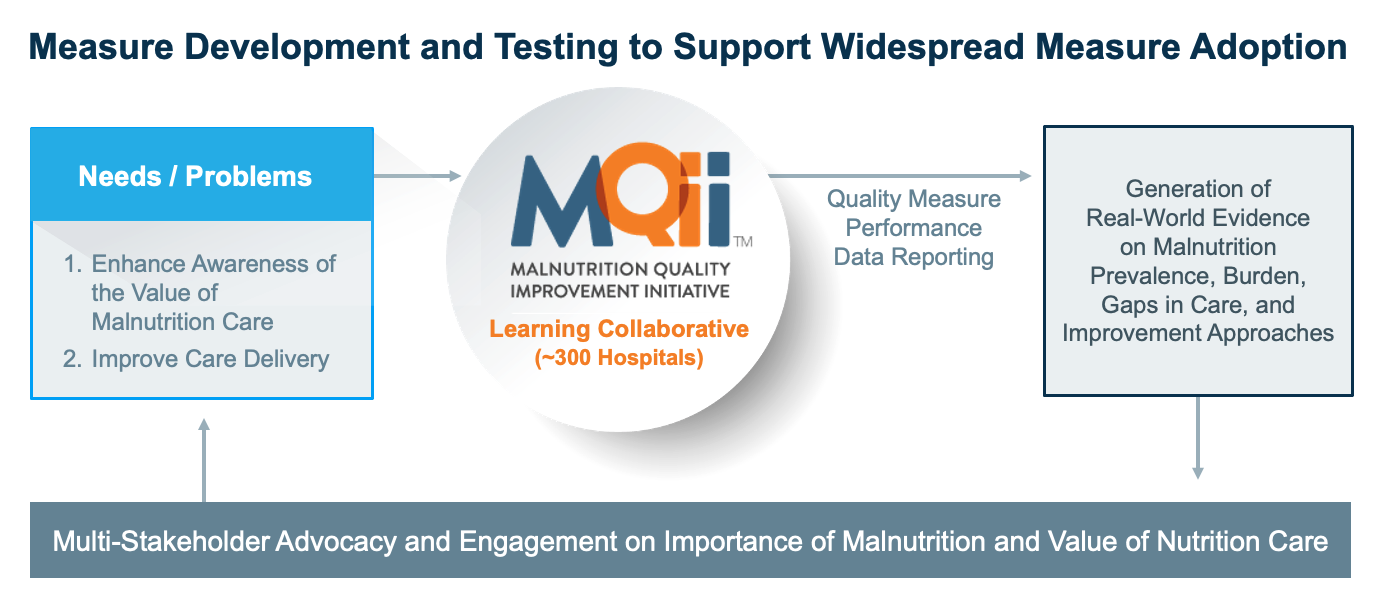
This promising announcement of support for the measure stems from a multi-year partnership with the Academy to establish and oversee the Malnutrition Quality Improvement Initiative (MQii). The MQii was established to raise awareness about the malnutrition care process and to generate real-world evidence on malnutrition care gaps and provider efforts to improve care from hospitals around the country via a national Learning Collaborative. The measure was tested through this Learning Collaborative and has now been adopted in hundreds of hospitals across the US to improve the care and outcomes for malnourished or at-risk patients. The success of this initiative was highly dependent on the contributions of the Academy, Learning Collaborative members, MQii’s advisory and technical expert panels, and other nutrition stakeholders who contributed their expertise.
MAP Recommends Conditional Support Pending NQF Endorsement
The MAP’s final recommendation of “Conditional Support Pending NQF Endorsement” follows extensive review by multi-stakeholder committees. These committees are convened by the NQF for healthcare quality experts to weigh in on measures the Centers for Medicare & Medicaid Services (CMS) proposes to adopt in its quality reporting and value-based care programs. The outcome of “conditional support” indicates that the committee supports the CMS adoption of this measure when an NQF committee of quality measurement experts endorses the measure for use. At the time, this NQF committee has already begun its review and has responded favorably to the evidence supporting the measure rationale and the measure’s feasibility, validity, and reliability. The committee will open for public comment in April 2021 and come to a final decision in June.
If the CMS moves forward with this recommendation, the measure would be slated for the IQR, with approximately 3,200 US hospitals reporting. Developed in 2003, the IQR is the longest-running and primary quality reporting program for hospitals overseen by the CMS. To date, no IQR measures focus on nutrition care or malnutrition, despite recent surveillance data reporting that as many as 8% of hospital discharges are coded with a diagnosis of clinical malnutrition. These same data demonstrate that malnourished patients are at a significantly higher risk for 30-day readmissions, mortality, longer length of stay, and higher hospital costs.
Real-World Evidence Strategy to Test the Measure and Advance High-Quality Care for Malnourished Adults
The Global Malnutrition Composite Score focuses on adults 65 years and older admitted to inpatient service who received care appropriate to their level of malnutrition risk or malnutrition diagnosis, if properly identified. The measure components have been used by hundreds of hospitals across the US participating in the MQii. This initiative seeks to advance evidence-based, high-quality, patient-driven care for hospitalized older adults who are malnourished or at risk for malnutrition. The growing membership of the MQii Learning Collaborative now comprises almost 300 hospitals that use a collaborative approach to support quality improvement (QI) implementation, use of the measure components to track and monitor progress, and better clinical outcomes for patients at risk of malnutrition.
In anticipation of the evidentiary needs required by the MAP and NQF committees, Avalere pursued a robust real-world-evidence generation strategy. Avalere collaborated with hospital participants to generate new evidence on the impact of malnutrition, best practices for closing care gaps, and resulting improvements in clinical outcomes. These data form 1 of the largest nutrition care datasets of its kind, including more than 1 million hospital encounters. These data allow Avalere and the health system participants to understand the prevalence and burden of malnutrition on hospital patients, where there are gaps in care for those at risk, and the impact of closing those gaps. Further, the data generated were used to evaluate the use of the developed measures and assess how they correlated with important outcomes of care.
Reflecting these efforts, Avalere co-authored several articles in peer-reviewed journals that include studies related to:
- Usability testing of an MQii Toolkit to support hospitals in implementing malnutrition-focused QI1,2
- Improvements in quality measure performance reported after QI implementation3,4
- Aggregate impact of measure implementation on clinical care and outcomes in a cohort of hospitals5
- Composite measure’s development methodology and results from reliability and validity testing6
- Use of the measure components in hospital subpopulations to assess their malnutrition burden7
Further, Avalere and the Academy released a joint special journal supplement highlighting more than a dozen abstracts and articles that demonstrate the value of improving malnutrition care and were authored by Learning Collaborative participants.
Broader Application
The lessons learned and experiences gained from this multi-year initiative may be applied to other areas in healthcare where similar barriers could be addressed by this real-world-evidence-focused approach. Such areas include:
- Lack of specific evidence demonstrating gaps in care
- Lack of provider engagement
- Insufficient care to address patients’ needs in specific care settings or specific medical specialties
- Poor compliance with evidence-based practices
- Little to no attention paid to certain therapeutic areas by federal and state governments or other public stakeholders
The prospect of support from the CMS to pursue malnutrition quality measures accelerated growth of the Learning Collaborative membership. The larger representation of hospitals facilitated real-world data generation, which supported measure testing, a better understanding of malnutrition best practices, and improving malnutrition care delivery and patient outcomes. The proliferation of value-based programs—whether in the form of quality reporting or innovative payment models—suggests this is an opportune time to implement approaches like these across other clinical areas and settings of care.
Further, the benefits of this program—such as improved collaboration across providers, implementation of standardized workflows, and support from senior health system leadership—may translate well to other areas of interest. Ultimately, the focus on improving the state of the evidence in malnutrition care has supported varied tactics that will improve the quality of care for patients across the healthcare environment.
Support for the MQii is provided by Abbott.
To receive Avalere updates, connect with us.
References
- Silver HJ, Pratt KJ, Bruno M, Lynch J, Mitchell K, and McCauley SM. Effectiveness of the malnutrition quality improvement initiative on practitioner malnutrition knowledge and screening, diagnosis, and timeliness of malnutrition-related care provided to older adults admitted to a tertiary care facility: a pilot study. Journal of the Academy of Nutrition and Dietetics. 2018;118(1):101–109. doi:10.1016/j.jand.2017.08.111.
- Nepple KG, Tobert CM, Valladares AF, Mitchell K, and Yadrick M. Enhancing identification and management of hospitalized patients who are malnourished: a pilot evaluation of electronic quality improvement measures. J Acad Nutr Diet. 2019;119(9 Suppl 2):S32–S39. doi:10.1016/j.jand.2019.05.023.
- Danis K, Kline M, Munson M, Nickleach J, Hardik H, Valladares AF, and Steiber A. Identifying and managing malnourished hospitalized patients utilizing the malnutrition quality improvement initiative: the upmc experience. J Acad Nutr Diet. 2019;119(9 Suppl 2):S40-S43. doi:10.1016/j.jand.2019.05.020.
- Pratt KJ, Hernandez B, Blancato R, Blankenship J, and Mitchell K. Impact of an interdisciplinary malnutrition quality improvement project at a large metropolitan hospital. BMJ Open Qual. 2020;9(1). doi:10.1136/bmjoq-2019-000735.
- Valladares AF, Kilgore KK, Partridge J, Sulo S, and McCauley SM. How a malnutrition quality improvement initiative furthers malnutrition measurement and care: Results from a hospital learning collaborative. Journal of Parenteral and Enteral Nutrition. 2020. doi:10.1002/jpen.1833.
- Wills-Gallagher J, Kirk KW, Macintosh B, Valladares AF, Kilgore KM, and Sulo S. Implementation of malnutrition quality improvement reveals opportunities for better nutrition care delivery for hospitalized patients. J Parenter Enteral Nutr. 2021. doi: 1002/jpen.2086.
- Valladares AF, McCauley SM, Khan M, D’Andrea C, Kilgore K, and Mitchell K. Development and evaluation of a global malnutrition composite score. Journal of The Academy of Nutrition and Dietetics. 2021. doi:1016/j.jand.2021.02.002.





