State Copay Accumulator Bans Will Affect 19% of US Commercial Lives
Summary
19% of people enrolled in the US commercial insurance market will belong to a health plan that must count copay assistance toward patient cost sharing by 2024.Note: This insight was originally posted on May 13, 2022. It was most recently updated on June 22, 2023, to include new information.
In recent years, payers and pharmacy benefit managers (PBMs) have increasingly used copay adjustment programs (i.e., copay accumulators and copay maximizers) to limit plan sponsor exposure to prescription drug costs. Manufacturers often offer patient copay assistance programs to commercially insured patients to reduce their out-of-pocket drug costs. Copay adjustment programs prevent this third-party assistance from counting toward patient’s deductibles and maximum out-of-pocket calculation as it otherwise would have without an adjustment program.
Research has shown that more than 83% of commercial market enrollees belong to plans that have implemented copay accumulator programs, and 73% belong to plans that have implemented copay maximizer programs. Recent federal rulemaking provided guidance for plans and payers to use these programs in broader insurance markets (e.g., large/small group, exchange) while also introducing challenges, such as the need for manufacturers to ensure that their financial assistance is passed fully through to patients.
Over the past several years, state legislators have passed bills aimed at banning the use of copay accumulator programs and ensuring that any third-party copay assistance used by a patient is counted toward the cost-sharing limits of that patient’s plan. As of June 2023, 19 states have enacted laws banning payer and PBM use of copay accumulator programs. These laws apply to state-regulated health plans, including the individual, fully insured large-group, and small-group markets. As of January 1, 2024, at least 19% of the total US commercial market—26.46 million individuals—will be enrolled in plans that must count any form of copay assistance toward patient cost-sharing limits. Additional states may enact laws as they wrap up their 2023 state legislative sessions, increasing this number.
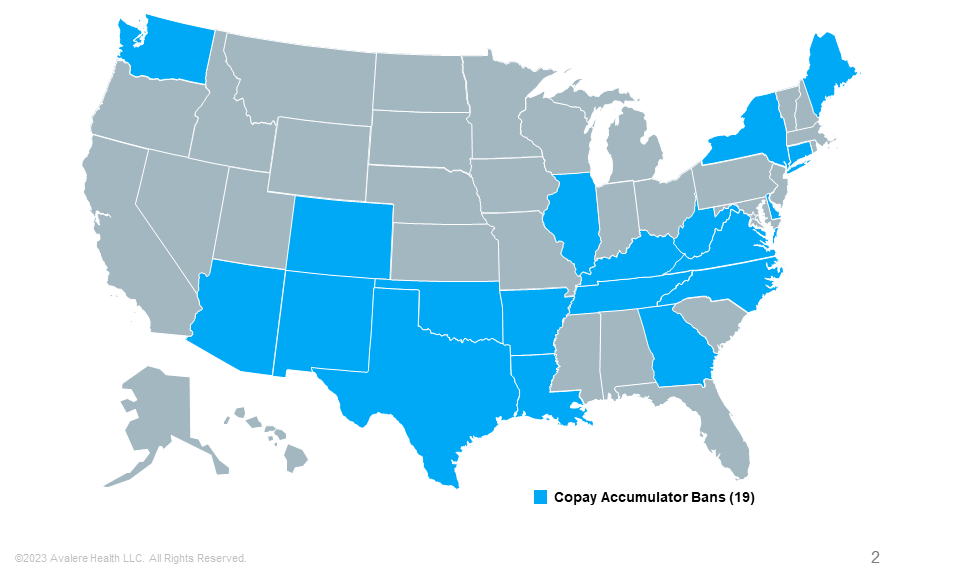
Note: State-level activity current as of June 21, 2023.
Puerto Rico has also enacted a copay accumulator ban.
Avalere Outlook
Avalere helps clients understand the evolving landscape of patient support, model the impacts of these policy changes, and identify solutions accounting for financial exposure while maximizing appropriate patient access. With its hands-on policy experience from the payer, manufacturer, and third-party vendor perspectives, Avalere is well positioned to help your organization respond to—or shape—the evolving copay adjustment program landscape.
To receive Avalere updates, connect with us.
| State | State-Regulated Covered Individuals (2019–2022) |
|---|---|
| Arizona | 876,118 |
| Arkansas | 551,240 |
| Connecticut | 550,427 |
| Colorado | 1,129,842 |
| Delaware | 124,215 |
| Georgia | 2,303,026 |
| Illinois | 2,670,903 |
| Kentucky | 497,133 |
| Louisiana | 714,202 |
| Maine | 303,775 |
| New Mexico | 219,048 |
| New York | 3,588,497 |
| North Carolina | 1,667,770 |
| Oklahoma | 769,161 |
| Tennessee | 1,097,155 |
| Texas | 5,689,603 |
| Virginia | 1,843,397 |
| Washington | 1,661,125 |
| West Virginia | 203,721 |
| Total Commercial State-Regulated Lives Under Copay Accumulator State Bans |
26,460,358 |
| Total US Commercial Lives | 19% |
Note: Puerto Rico has also implemented a copay accumulator ban; these numbers do not account for non-Employee Retirement Income Security Act (ERISA) covered lives as part of this analysis.
Sources: Kaiser Family Foundation, “Marketplace Enrollment, 2014–2023”; Kaiser Family Foundation, “Market Share and Enrollment of Largest Three Insurers – Large Group Market, 2019“; Kaiser Family Foundation, “Market Share and Enrollment of Largest Three Insurers—Small Group Market, 2019“; AHIP, “Health Coverage: State-to-State, 2023.”







