White-Bagging Legislation Gains Popularity in State Legislatures
Summary
In recent years, payers and pharmacy benefit managers (PBMs) have been interested in implementing strategies that may reduce overall costs, such as the use of white bagging. However, provider and patient groups have raised concerns that these tactics may create access to care, cost, and safety issues. Legislation seeking to regulate this practice is on the rise in many state legislatures.White bagging occurs when a payer or PBM requires insurance coverage of a patient’s physician-administered prescription drug to be dependent on a physician receiving the products from a payer or PBM-selected pharmacy (often a specialty pharmacy). The physician is reimbursed the drug’s administration fee under the medical benefit, while the pharmacy collects the copayment or coinsurance from the patient and reimbursement from the issuer under the patient’s pharmacy benefit. In contrast, physicians traditionally use a buy-and-bill model, where the provider purchases, stores, and administers a drug to a patient, then is reimbursed by the patient’s payer for both the drug administration and the drug itself under the medical benefit.
Payers and PBMs note that white bagging may provide cost savings that can be passed on to patients. However, provider groups have raised safety concerns over the implementation of white bagging, such as delays in the administration of medication caused by shipping or storage factors and delays in accessing care if the medication is not readily on hand at a provider’s office. Provider groups also argue that when patients require a change in dosage, strength, or class of medication, white bagging can lead to waste because the already dispensed medication cannot be used for a different patient. Patient advocates have also cited that white bagging could change where patients receive medications (e.g., outpatient facilities) and alter patient out-of-pocket costs due to shifts in the pharmacy versus medical benefit.
Current State Legislative Activity
While federal action on white bagging is limited, state legislatures are increasingly focused on regulating PBMs and issuers in 2022. Specifically, state legislators are introducing white-bagging bills aimed at prohibiting payers and PBMs from mandating provider/patient uses specific pharmacies for provider-administered drugs as a condition of reimbursement or patient coverage. In 2021, 3 states enacted white bagging laws (AR, LA, VA). Keeping with this trend, at least 10 states are actively considering white-bagging legislation so far in 2022. 2 additional states (FL, WI) considered white-bagging bills that ultimately failed in committee. Of these 10 states, at least 2 (WV, OK) have passed their bill through at least 1 legislative chamber.
The states’ increased interest in white-bagging bills and consequently the regulation of payers and PBMs may be due to the Supreme Court’s 2020 ruling in Rutledge v. PCMA. The ruling found that the Employee Retirement Income Security Act does not necessarily preempt state laws regulating healthcare costs, creating an opportunity for states to regulate PBM business practices that manage benefits on behalf of employers. Since this decision, state legislators have noticeably increased the number of proposed bills aiming to regulate PBMs, including white-bagging bills.
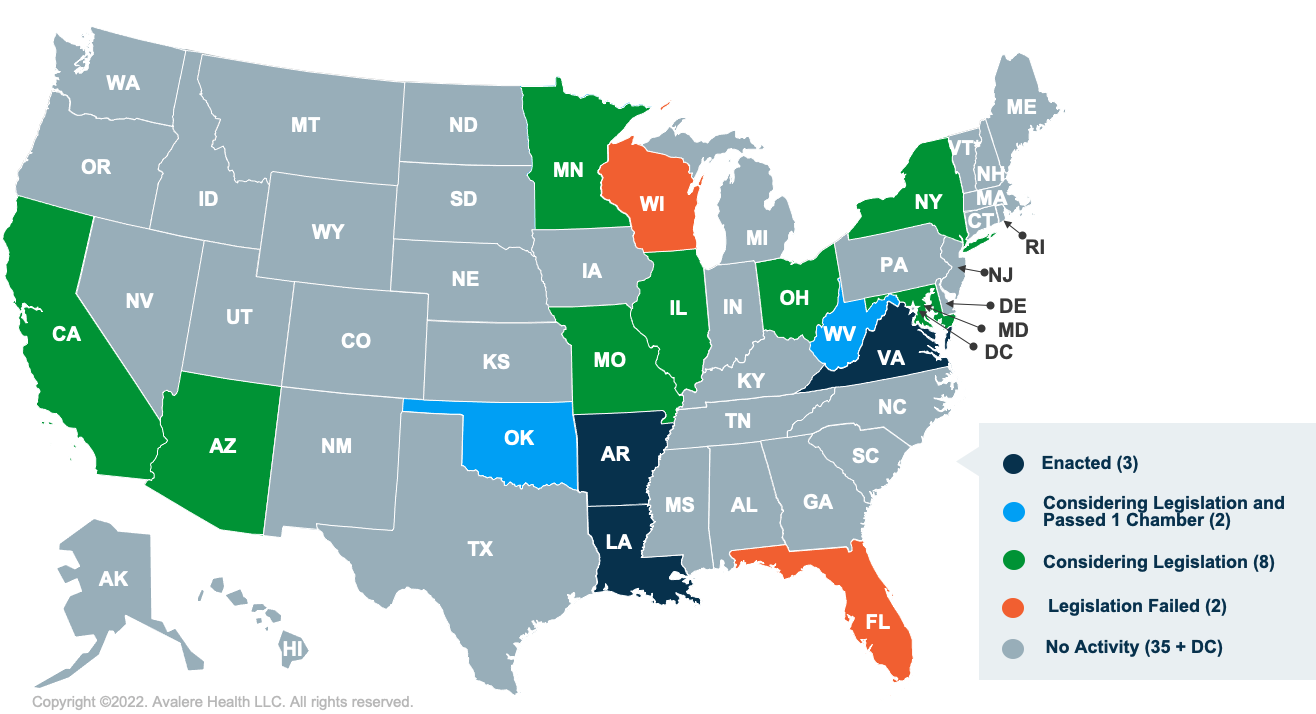
Note: This map reflects bills actively considered in 2022 and laws that were enacted prior to 2022, as of April 21, 2022. Source: State Policy 360.
Given the increased state legislative activity so far in 2022, it is likely additional states will enact laws related to white bagging this year. These laws could have a substantial effect on how provider-administered products are administered, site of care barriers, and patient access to care such as unexpected financial considerations. Further, patient advocacy groups cite increased safety concerns over white bagging, including how many physician-administered products are tailored to a patient and may need special handling. As these bills have important considerations for stakeholders across the industry, remaining up to date on and analyzing patterns in state white bagging legislation may help industry leaders to proactively respond to state activity that impacts their firm’s operations.
To learn more about how we track and analyze emerging state issues, check out State Policy 360TM. Stay ahead of emerging state policy activity. Monitor what’s important for your business across all 50 states and DC, and see major trends in Medicaid waivers, drug benefit management, prescription drug pricing, health equity, and individual market changes.
For more on drug pricing trends and news, connect with us.
January 23, 11 AM ET
Learn More



