Avalere Analysis Shows that Health Needs and Cost of Medicaid Expansion Populations Grow over Time
Summary
Beneficiaries show signs of pent-up demand with acute healthcare needs early in their enrollment, but over time costs increase substantially and shift toward chronic care.A new analysis from Avalere Health finds that healthcare spending for the Medicaid expansion population increased steadily over time for beneficiaries who remained enrolled in the program. The enactment of the Affordable Care Act (ACA) provided states with the option of extending Medicaid eligibility status to childless adults aged 19-64 who earn less than 138% of poverty ($16,643 for an individual), many of whom were previously uninsured.
Avalere’s research shows that average monthly costs for expansion enrollees who gained coverage in the first half of 2014 were $324 during the first 6 months of coverage and rose to $389 for those who were still enrolled two and a half years later (months 31 through 36), a 20% increase (Figure 1). The analysis also found that younger enrollees are more likely to disenroll over time, leading Avalere experts to conclude that healthier enrollees may be disenrolling or losing Medicaid eligibility, while expansion enrollees with sustained enrollment in the program are more likely to have chronic health needs.
“Contrary to some expectations that Medicaid expansion enrollees would be relatively healthy, beneficiaries who have remained on the program have increasing healthcare needs, likely due to previously unidentified or untreated conditions,” said Caroline Pearson, senior vice president at Avalere. “Healthier, lower-cost enrollees may be more likely to churn off Medicaid after a shorter period of time.”
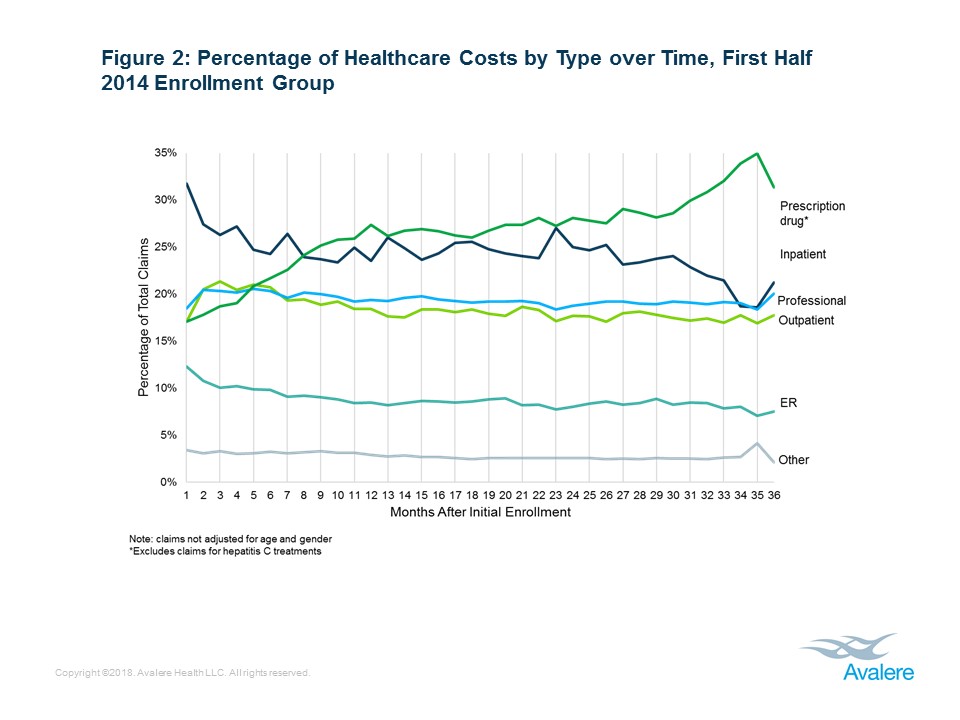
Inpatient Costs Drop Dramatically Over Time While Prescription Drug Spending Grows
Avalere also analyzed healthcare spending by type of service, and found that the share of spending for inpatient hospital care and emergency room (ER) visits decreased over time, especially in the first few months of coverage, while spending for chronic care services, such as prescription drugs, increased over the study period (Figure 2). Among those enrolled in early 2014, inpatient spending initially made up the largest share of costs, but was surpassed by prescription drug spending by month 8 of enrollment.
Avalere experts observe that high rates of initial inpatient and ER use suggesting that expansion enrollees, largely uninsured prior to 2014, had significant medical needs upon enrollment, or that many expansion enrollees enrolled as a result of an inpatient encounter. However, as beneficiaries spend more time with comprehensive insurance coverage and establish relationships with physicians, their healthcare costs shift toward outpatient visits and prescription drugs-a core component of chronic disease treatment-and away from hospitalizations, which reflect acute health needs.
The study showed that pharmacy costs (excluding Hepatitis C) almost doubled over the two and a half year time period that the initial cohort was tracked. This is likely an indication that the previously uninsured population may have had untreated conditions and gaining access to health insurance helped provide needed care to these enrollees.
“As new Medicaid beneficiaries gain a consistent and sustained source of insurance coverage, their spending patterns reflect improved care for chronic conditions and less need for acute hospitalizations,” said Michael Lutz, vice president at Avalere. “This suggests that newly insured populations have underlying health needs but insurance coverage may help rationalize their healthcare spending in favor of longer-term, less costly treatments overall.”
The complete analysis is available here.
Methodology
Avalere received claims data from January 2014 through December 2016 from three Medicaid managed care organizations (MCOs) offering coverage in states that expanded Medicaid on January 1, 2014. In total, their data represented nine unique state-plan combinations. Medicaid expansion enrollees were defined as individuals who gained eligibility due to the state’s decision to expand coverage under the ACA. Membership in each plan was categorized into 6-month period enrollment groups based on the initial enrollment date (e.g., an individual that enrolled between January and June 2014 was included in the “first half 2014” enrollment group).
Claims data included both medical and pharmacy claims but exclude prescription drug claims for Hepatitis C treatments. Services paid for on a sub-capitated basis were also excluded from the analysis. Except where noted in the category of service analysis, claims data were normalized by both age and gender to negate the effect of age or gender influences on the change in claims over time (i.e., duration or incurred period). The age/gender normalization factors were derived from a state’s most recently available state pricing or expected claims costs for the expansion population. The claims were also adjusted for any material program changes (e.g., benefit changes, fee schedule changes) through 2016.
Funding for this analysis was provided by the Anthem Public Policy Institute. Data were provided by several Medicaid managed care organizations. Avalere maintained full editorial control.