Medicare Patients Are Using Fewer Skilled Nursing Services
Summary
New research from Avalere finds Medicare beneficiaries are spending fewer days in skilled nursing facilities (SNFs) since 2009 on a per capita basis.Based on Avalere’s analysis, the decline appears to be driven by changing patterns of inpatient hospital care, including fewer hospital inpatient admissions and more frequent observation stays, which result in fewer discharges to SNFs.
Following hospitalizations for injury or illness, many patients are discharged to a post-acute care (PAC) facility, where they can continue their recovery or manage their illness. In a SNF—one of four types of PAC facilities—clinicians provide a range of services, including physical therapy, occupational therapy, and speech therapy. The Medicare program covers up to 100 days of SNF care for eligible stays. To qualify for treatment in a SNF, a patient must have at least three days of care in an inpatient hospital prior to being admitted to the SNF. However, if a patient is admitted to the hospital for observation rather than an inpatient stay, they will not be eligible for a SNF following discharge.
“The economics of post-acute care have been fundamentally changed as Medicare shifts its payment approach to capitation, bundles, and pay for value,” said Dan Mendelson, president at Avalere. “Fewer patients are being admitted to the hospital, as payers and risk-bearing providers seek to shift care to lower-cost settings.”
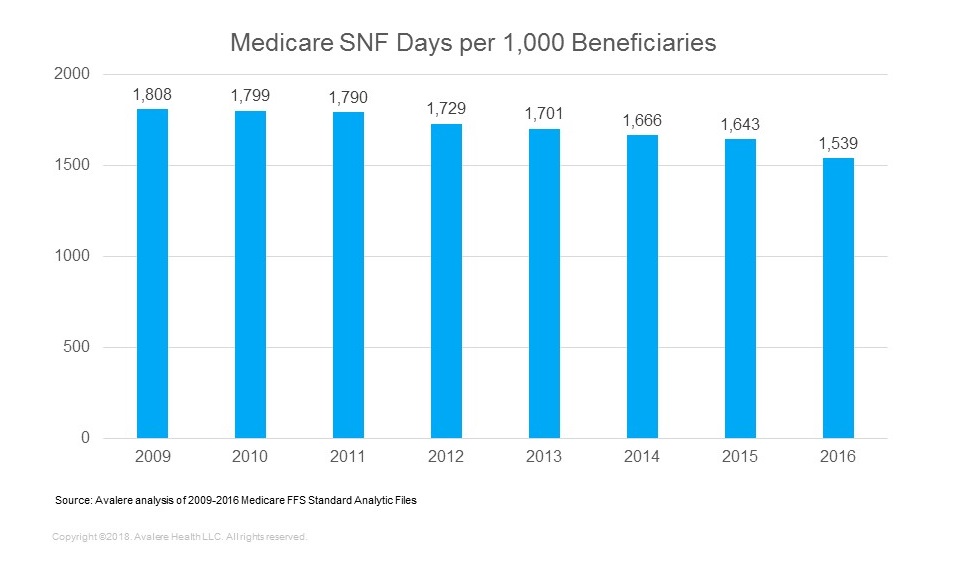
Based on Avalere’s analysis of beneficiaries in traditional fee-for-service (FFS) Medicare, SNF utilization has declined every year since 2009, when there were 1,808 SNF days per 1,000 Medicare fee-for-service (FFS) beneficiaries compared to only 1,539 in 2016—a 15% decline (Figure 1).
“The long-term erosion in hospitalizations contributes directly to the decline in SNF utilization among Medicare beneficiaries,” said Fred Bentley, vice president at Avalere Health. “While hospitals that are aggressively moving to value-based payment are shifting discharges from SNFs to home health providers, the biggest driver of the decline in SNF use appears to be the reduction in hospitalizations.”
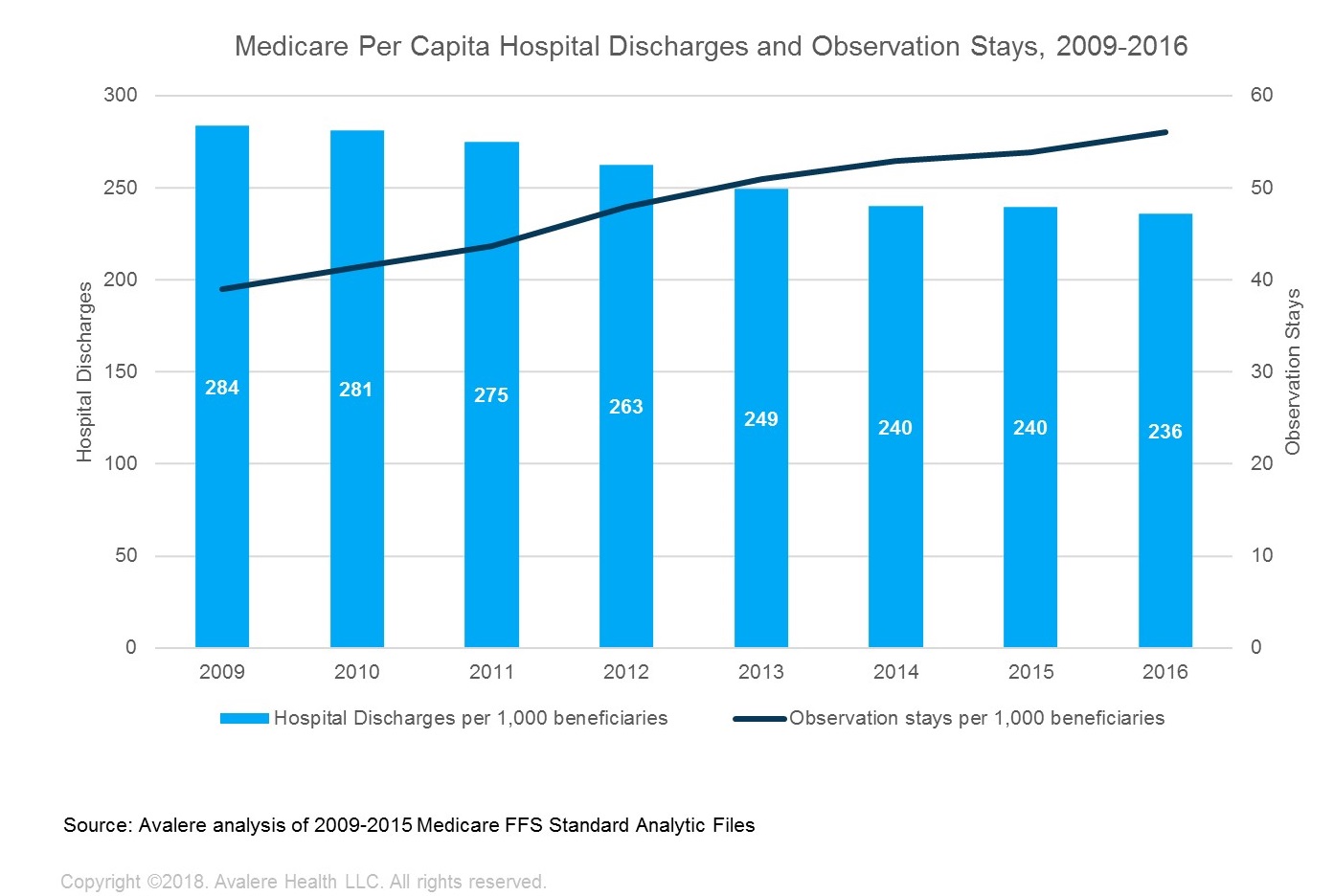
Avalere’s analysis found that since 2009, per capita hospital discharges have declined 17%, concurrent with an increase in observation stays (Figure 2). Observation patients are typically treated in a hospital but are lower-acuity cases that require observation before they are discharged. Avalere experts suggest that payment models that penalize readmissions and scrutiny of short inpatient stays may be driving more frequent use of observation stays.
According to Avalere experts, in addition to inpatient hospital discharges, SNF utilization can also be affected by changes in discharge patterns among different types of post-acute care facilities (e.g., SNF, home health agencies, inpatient rehabilitation facilities, long-term acute care hospitals), and average length of stay for patients in a SNF. Avalere experts did not observe shifts in the proportion of discharges to SNFs relative to home health and other PAC settings, and average SNF length of stay remained stable at about 24 days since 2009. These findings suggest that inpatient volumes are driving the reduction in SNF use.
“Over the past few years, fewer beneficiaries are being admitted to skilled nursing facilities,” said Erica Breese, director at Avalere. “Continued population growth is expected to counteract the utilization declines, but there appears to be a steady shift in how Medicare beneficiaries are using inpatient services and skilled nursing care.”
Methodology
Avalere calculated national inpatient hospital discharges and observation stays, as well as skilled nursing facility admissions and length of stay for 2009 through 2016. Avalere identified utilization using adjudicated Medicare fee-for-service claims submitted to the Centers for Medicare & Medicaid Services (CMS) from the CMS Standard Analytic Files (SAFs), which include 100% Medicare fee-for-service Part A claims. In order to calculate per capita utilization, Avalere used CMS’ enrollment file to calculate the number of beneficiaries enrolled in FFS at any point during the year.
Funding for this research was provided by Omega Healthcare Investors, Inc. Avalere maintained full editorial control.
To receive more expert insights on SNF trends and issues, connect with us