SNF 3-Day Waiver Use During the COVID-19 Pandemic
Summary
Use of the 3-day waiver was stable over the course of the pandemic, though shifts in admission sources were observed.Effective March 1, 2020, the Centers for Medicare and Medicaid Services (CMS) temporarily waived the 3-day inpatient hospitalization requirement for Medicare-covered skilled nursing facility (SNF) stays. This waiver allowed beneficiaries to receive Medicare-covered SNF care without a prior hospital stay of at least 3 days. It expired with the end of the federal public health emergency (PHE) on May 11, 2023.
The 3-day inpatient stay requirement for Medicare-covered SNF stays has been discussed by policymakers for years, even prior to the COVID-19 pandemic. Several CMS initiatives have waived this requirement, such as certain accountable care organization programs and the Bundled Payment for Care Improvement initiative. In non-PHE contexts, policymakers have considered whether a 3-day stay waiver could lead to increased SNF stays in the absence of current requirements.
The PHE was the first time the waiver had been applied more broadly, offering an opportunity to examine its potential for wider use.
Waiver Use and COVID-19 Status
Avalere analyzed claims for all SNF stays from March 2020 to December 2021 and the use of the 3-day waiver among beneficiaries without a diagnosis for COVID-19 (i.e., non-COVID) as the pandemic subsided.
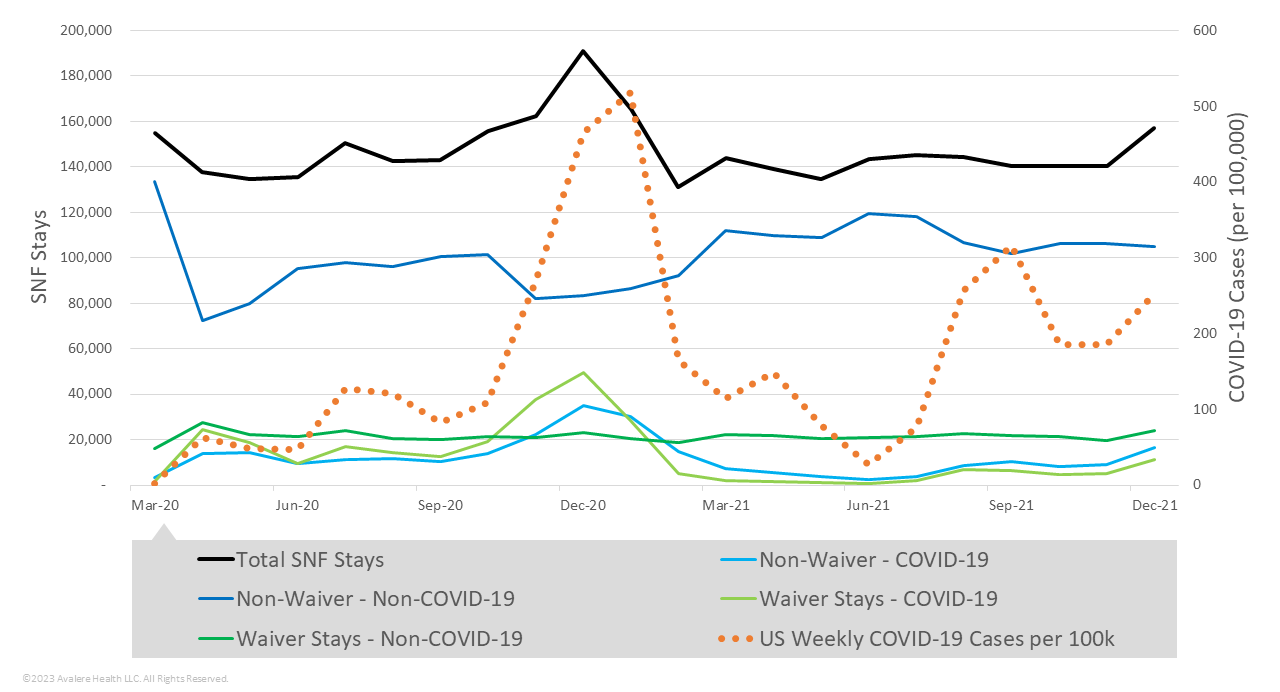
Utilization of the 3-day waiver generally aligned with COVID-19 case rates. Non-COVID waiver stays remained at approximately 15% of total SNF stays throughout the pandemic (Figure 1).
Sources of Admissions
Avalere also analyzed the sources of admission for 3-day waiver stays to identify trends in utilization prior to and following the availability of COVID-19 vaccinations (Figure 2). In 2020, 45% of non-COVID 3-day waiver stays (6.5% of total SNF stays) were admitted from nursing facilities. Medicare beneficiaries initiating SNF stays from nursing facilities may have been long-term nursing home residents in need of higher-level care due to an acute medical need. In many cases, the same provider cared for these beneficiaries, but the reimbursement shifted to Medicare.
In 2021, the highest proportion of 3-day waiver stays were admitted following inpatient hospitalizations of fewer than 3 days. Additionally, the proportion of beneficiaries using the 3-day waiver who were admitted from nursing facilities decreased notably (from 12% of total SNF stays in April 2020 to 3% in April 2021). This change corresponds with the drop in COVID-19 weekly cases following the early distribution of COVID-19 vaccinations to nursing facility residents.
Figure 2. Non-COVID-19 3-Day Waiver Stays, by Admission Source
Primary Diagnosis and Source of Admission
SNF patients are classified into one of ten Patient Driven Payment Model (PDPM) clinical categories based on the primary diagnosis for the SNF stay. The PDPM condition category for 3-day waiver stays varied by admission source (Figure 3). The most common condition categories for patients admitted from the hospital setting (i.e., inpatient, emergency room, or observation) were medical management, acute neurologic, and non-surgical orthopedic or musculoskeletal conditions. These condition categories were consistently among the top three in 2020 and 2021.
In 2020 and 2021, the most frequent condition categories among 3-day waiver stays admitted from a physician’s office (from the community) were medical management and major joint replacement or spinal surgery. Medical management and acute neurologic were the most common condition categories for 3-day waiver stays admitted from nursing facilities in both 2020 and 2021, though the proportion of stays were higher for medical management in 2020.
Figure 3. Non-COVID-19 3-Day Waiver Stays, by Admission Source and PDPM Condition Category
Pandemic-Era Patterns
The relatively constant use of the 3-day waiver throughout the pandemic, alongside changes in use by admission source and condition categories tracking with COVID-19 case rates and vaccine availability, suggest that use of the 3-day waiver reflected the pandemic environment. As the vaccine became available and COVID-19 case rates decreased, direct transfer to Medicare-covered SNF stays from nursing facilities decreased. Overall, SNF stays remained relatively stable over the time period of this analysis with slight increases corresponding to COVID-19 case rates.
Additional analyses using 2022 data will further inform policy discussions regarding 3-day waiver availability more broadly and its potential to impact efficiency in care delivery and quality of care.
Funding for this research was provided by the American Health Care Association. Avalere retained full editorial control.
To learn more about Medicare policy, connect with us.
Methodology
Avalere used the 100% Medicare fee-for-service claims data to analyze SNF stays from March 2020 through December 2021. Claims data were accessed via a research collaboration with Inovalon, Inc., and governed by a research-focused CMS data use agreement. Waiver stays were identified by a condition code signifying the 3-day waiver (condition code = DR). In cases where SNF stays were coded as waiver but had prior inpatient stays of 3 days or more, Avalere recoded waiver status to non-waiver for this analysis as these reflect Medicare-covered SNF stays under current law. SNF stays for patients treated for COVID-19 were identified based on the presence of International Classification of Diseases (10th revision) diagnosis code U071 (COVID-19).






