States Mitigate Potential Coverage Losses Ahead of ACA SCOTUS Ruling
Summary
With the US Supreme Court (SCOTUS) set to hear arguments starting November 10 in California v. Texas and the swearing in of Justice Amy Coney Barrett on October 26, questions remain regarding the future of the Affordable Care Act (ACA) and its impact on laws passed in at least 18 states creating coverage protections for essential health benefits (EHB) and coverage of pre-existing conditions.California v. Texas concerns the constitutionality of the ACA following Congress’s decision to set the individual mandate penalty to $0 in the 2017 Tax Cuts and Jobs Act. In January, the US House of Representatives and Democratic attorneys general filed a motion asking the SCOTUS to review the 5th Circuit’s December 2019 ruling that the individual mandate is unconstitutional. Though the SCOTUS denied a motion to expedite California v. Texas during its last term, it agreed to schedule oral arguments in the case on November 10. A ruling is expected by June 2021. Additionally, many believe that the addition of Justice Amy Coney Barrett creates a largely conservative Court, which stakeholders have expressed could impact the decision of California v. Texas
Following passage of the ACA, many states took steps to extend certain protections to their insurance markets. However, states vary widely as to which protections they have codified in their laws. Importantly, how some states have codified these protections (e.g., by referencing federal law in state law) may be impacted if the ACA is ultimately invalidated in California v. Texas. Stakeholders are concerned about the potential for coverage disruption due to possible invalidation of the ACA. While some of the ACA’s market reforms apply to self-insured employer-sponsored plans, any changes to state laws will apply only to individual and group insurance in the state. Notably, under the ACA, EHB do not apply to self-insured employer-sponsored plans.
Recent State Responses
Several states are seeking to enact statewide protections in their own laws that are specifically designed to guard against the possibility of the ACA being invalidated in California v. Texas. Protections focus on pre-existing condition exclusions, coverage without cost sharing for preventive services, guaranteed issue, and coverage for select or all EHB (e.g., prescription drug coverage, mental health, substance use disorder services).
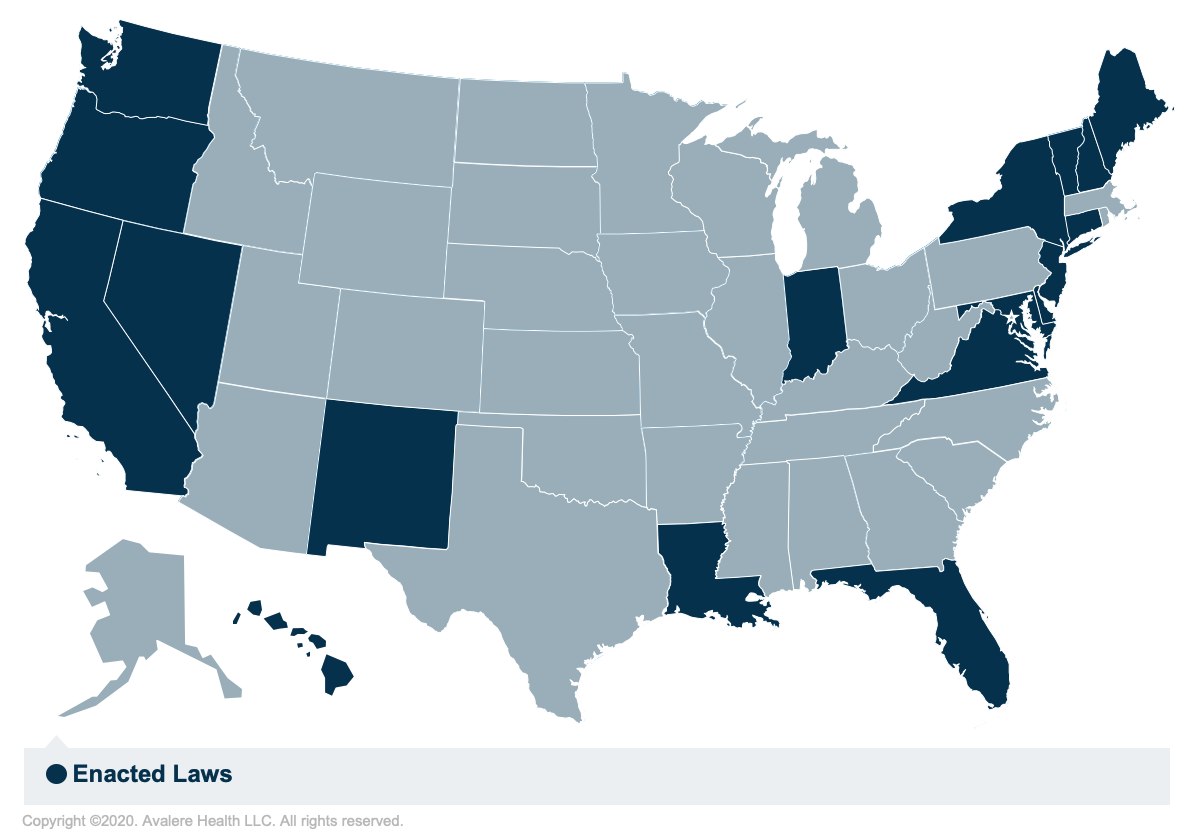
In 2019 and 2020, at least 18 states (CA, CT, DE, FL, HI, IN, LA, MD, ME, NH, NJ, NM, NV, NY, OR, VA, VT, and WA) enacted laws with language to establish protections against pre-existing condition exclusions or coverage of all EHB provided for in the ACA. By defining these coverage requirements in statute and removing explicit references to the ACA, states could maintain the authority to regulate coverage of EHB and other ACA provisions, even if invalidated in California v. Texas. These efforts parallel other legislative trends across the country intended to ensure access to and affordability of coverage, such as the public option efforts in CO and WA and the individual mandate in CA, DC, MA, NJ, RI, and VT. Notably, some of these enacted laws and bills under consideration are written such that the protections would only become effective if the ACA is invalidated.
Regardless of state approaches to these protections, however, a loss of federally funded subsidies (e.g., cost-sharing reductions, advance premium tax credits) and federal funding for reinsurance programs could significantly hinder states’ ability to support the same levels of coverage for beneficiaries.
Conclusion
The outcome of California v. Texas is likely to have far reaching impacts for healthcare coverage in all states. Depending on the outcome of the case, state legislatures may need to act quickly to mitigate potential coverage losses.
To receive Avalere updates, connect with us.