Avalere Analysis: Exchange Enrollment Outpaces Expectations in 22 States
Summary
Analysis assumes 85 percent of enrollees pay first month's premium.A new analysis from Avalere Health finds that exchange enrollment meets or exceeds expectations in 22 states (44%), even after accounting for any attrition due to nonpayment of premiums. Assuming 15 percent of enrollees do not take the final enrollment step and pay their premiums, over 6.8 million people who enrolled through April 19 will have coverage effective as of May 1.
“The large uptick in enrollment in March and early April brought many states over the finish line in terms of projected enrollment for 2014,” said Caroline Pearson, Vice President at Avalere. “Even after accounting for potential non-payment, enrollment exceeds 100 percent of projections in nearly half of states.”
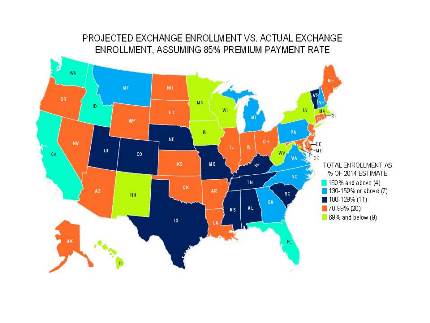
Avalere’s analysis compares exchange participation at the end of open enrollment to state projections based on the Congressional Budget Office (CBO) estimate that 6 million people would enroll in exchanges. Florida, California, and Idaho lead in enrollment compared to expectations, while Hawaii and the District of Columbia lag behind with less than 50 percent of expected enrollees paying their first month’s premium.
“Once again, the data paint a diverse and complex picture. Enrollment significantly beat expectations in some states but fell short in others,” said Elizabeth Carpenter, Director at Avalere. “Regional variation is a key feature of the current exchange marketplace, and it could impact carrier decisions to participate in some markets in 2015.”
Methodology
:
Avalere’s analysis incorporates the HHS enrollment figures released on May 1, 2014, as well as updated state-specific tracking from publicly-available resources in Colorado, Minnesota, and Oregon. Enrollment projections are based on Avalere’s projections for enrollment distribution by state at the end of 2014 applied to the CBO’s February enrollment projection of 6 million. This approach assumes smooth implementation across states; that is, eligible populations take up coverage at similar rates across states.
Since enactment of the Affordable Care Act (ACA), Avalere has developed and continually refined an enrollment model that projects coverage over ten years at the state level. The model accounts for state decisions about whether to expand Medicaid. In addition to enrollment reports from the federal government, Avalere utilizes a range of data sources to account for local population demographics and experience. Such sources include data from the Congressional Budget Office (CBO), Centers for Medicare & Medicaid Services (CMS) on Medicaid Managed Care Enrollment Report and Medicare Enrollment, the Census Bureau’s American Community Survey (ACS) and Current Population Survey (CPS), and the Urban Institute. Avalere also evaluates past program launches including the Medicare Part D Program and the Massachusetts exchange, known as the Health Connector.
For exchanges specifically, our model primarily examines local coverage and demographic information for the exchange-eligible population, which primarily includes the uninsured and non-group markets pre-2014. We also include some other modest shifts such as those out of employer coverage and those in states that previously had more generous Medicaid programs, planning to roll back eligibility to 138% of poverty and move these lives into the exchanges. Avalere assumes that seven states-Connecticut, Maine, New Jersey, New York, Rhode Island, Vermont, and Wisconsin-are shifting higher-income, adult Medicaid beneficiaries out of their Medicaid programs and into exchange coverage. It is unclear how quickly these states are making this transition, which could make the enrollment projections for these states appear higher than expected.
Avalere assumes 85 percent of people who choose a health plan will effectuate coverage by paying their first month’s premium, based on public comments by health insurers participating in the exchange which have indicated that 80 to 90 percent of applicants are paying premiums.
View the full press release attached.
For more information, contact Caroline Pearson at CPearson@Avalere.com.



