Avalere Analysis of Disparities in Kidney Care Service Utilization
Summary
In light of proposed changes to the ESRD Treatment Choices Model to address health disparities, an Avalere analysis of Medicare claims found gaps in access to and utilization of specific dialysis-related services by patient race, ethnicity, and socioeconomic status.On July 1, the Centers for Medicare and Medicaid Services (CMS) released the End-Stage Renal Disease (ESRD) Prospective Payment System (PPS) Calendar Year 2022 Proposed Rule. This rule proposes updating payment rates for renal dialysis services furnished to Medicare fee-for-service (FFS) beneficiaries starting January 1, 2022. This rule also includes proposed modifications to the ESRD Treatment Choices (ETC) Model, which was finalized in September 2020 and went into effect in January 2021. The ETC Model is a mandatory payment model intended to incentivize home dialysis and transplant growth among Medicare beneficiaries with ESRD through adjusted payments to selected ESRD facilities and managing clinicians.
Significant disparities exist in both healthcare outcomes and access to treatment among patients with kidney disease. If finalized, the proposed changes to the ETC Model would represent the Innovation Center’s first model to directly address health and socioeconomic disparities. The CMS has proposed a “Health Equity Incentive” to the model’s improvement score methodology; participants who improve rates of home dialysis and transplant among beneficiaries who are dually eligible for Medicare and Medicaid or are Low-Income-Subsidy (LIS) recipients would potentially earn additional improvement score points. The CMS has further proposed stratifying achievement benchmarks by the proportion of beneficiaries who are dually eligible for Medicare and Medicaid or LIS recipients to protect participants with a high volume of these patients from potential downside losses.
Avalere’s Analysis of Disparities in Access to Care
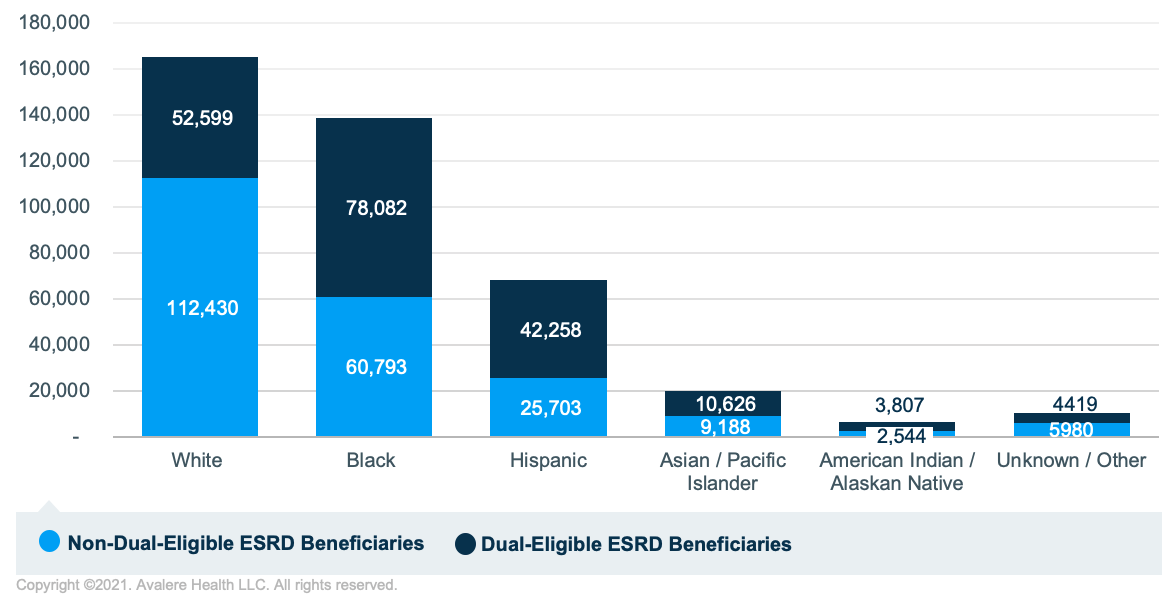
Avalere investigated the utilization of 3 discrete services, given their relevance to the ETC Model and kidney care more generally: kidney transplantation, home dialysis, and in-center dialysis. Avalere identified 408,429 Medicare FFS beneficiaries with ESRD in 2019 who met inclusion criteria. Of those beneficiaries, 40% were identified as White, 34% were Black, and 17% were Hispanic. Across the population as a whole, 47% were dual eligible (i.e., patients had both Medicare and Medicaid coverage), and a higher percentage of Hispanic and Black beneficiaries were dual eligible (62% of Hispanic ESRD beneficiaries and 56% of Black ESRD beneficiaries), while a lower percentage of White ESRD beneficiaries were dual eligible (32%; Figure 1).
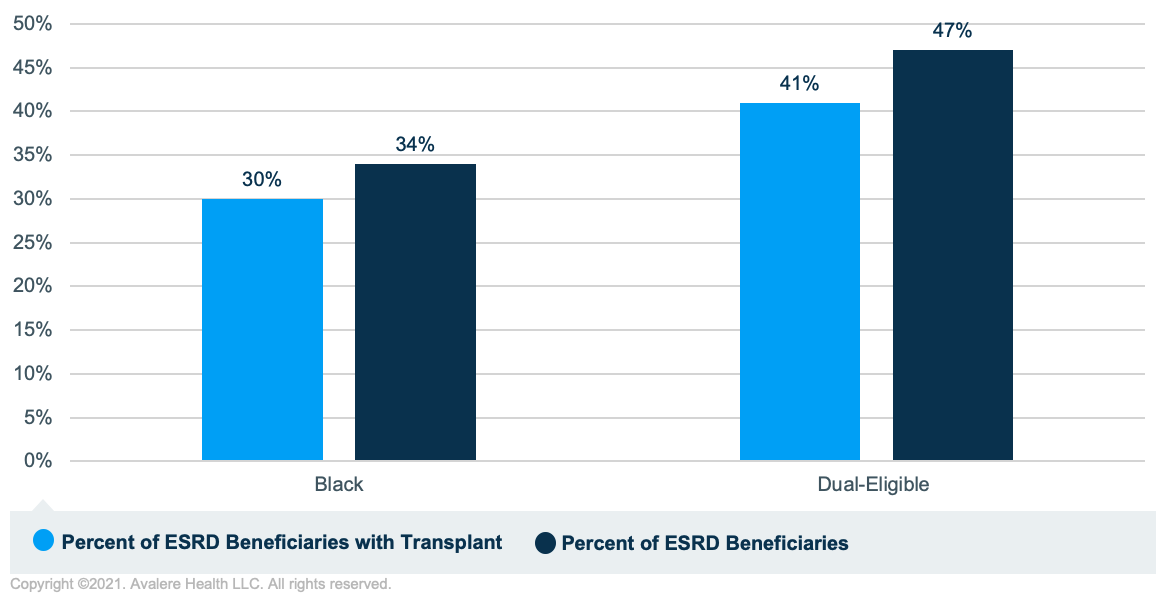
Transplants were rare events among the total population of beneficiaries with ESRD, and a disproportionately small percentage of transplant recipients were dual eligible. Similarly, a disproportionately small percentage of transplant recipients were Black (Figure 2). In 2019, only 3% of the Medicare FFS population with ESRD had a transplant, and fewer transplant recipients were dual eligible than the population as a whole (41% of transplant recipients were dual eligible while 47% of the population was dual eligible). A disproportionately low percentage of dual-eligible ESRD beneficiaries with a transplant were Black (35%) compared to the total percent of dual-eligible ESRD beneficiaries in the sample that were Black (41%). A higher percentage of dual-eligible ESRD beneficiaries with a transplant were Hispanic (27%) compared to the percentage of dual-eligible ESRD beneficiaries in the sample that were Hispanic (22%). This is compared to White beneficiaries, who comprised 27% of dual-eligible beneficiaries with ESRD and 26% of dual-eligible beneficiaries with both ESRD and a transplant.
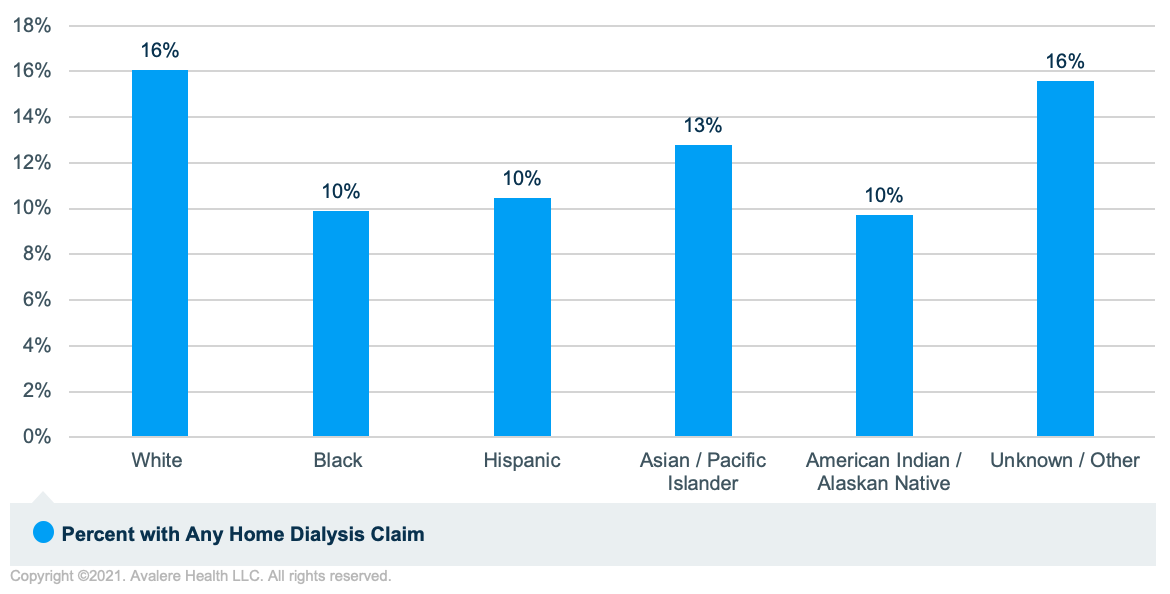
Less than 30% of the 408,429 FFS beneficiaries with ESRD had any home dialysis claims and, among minority groups (dual-eligible, Black, and Hispanic beneficiaries), the percentage with home dialysis claims was even lower. Of the total sample, 8% received home dialysis only, 5% had received both home and in-center dialysis (13% with any home dialysis claims), and 71% received in-center dialysis only. A lower percentage of dual-eligible ESRD beneficiaries had home dialysis claims (10%) compared to non-duals (15%). Likewise, a lower percentage of Black (10%) and Hispanic (10%) ESRD beneficiaries had home dialysis claims compared to White ESRD beneficiaries (16%; Figure 3).
Separately, pre-dialysis education is critical among patients with chronic kidney disease (CKD) to inform patients of their treatment options, slow the progression of the disease, and support optimal dialysis starts among those who transition to ESRD. Medicare currently covers up to 6 kidney disease education (KDE) sessions under Part B for beneficiaries with Stage 4 CKD, and there is consensus among stakeholders that KDE provides a meaningful opportunity to address disparities in modality selection, general awareness of the disease, and comorbid management. Still, since its establishment in 2010, utilization of the KDE benefit has been extremely limited. Among Avalere’s analysis of over 25 million beneficiaries receiving outpatient care in 2019, KDE billing codes were only identified for 139 beneficiaries
As part of the latest proposed rule, the CMS is considering waiving certain requirements to support expanded uptake of the KDE benefit within the ETC Model. These proposals include waiving the 20% coinsurance requirement and the geographic and site of care requirements to allow KDE to be furnished via telehealth. It will be important for the CMS to not only support expanded uptake of the KDE benefit but also to ensure its equitable access.
Opportunities for Stakeholder Action
Stakeholders in the kidney care space—including dialysis organizations, nephrologists, payers, and life sciences companies—can support the effort to close gaps in healthcare access and outcomes by understanding the clinical and social needs of historically underserved patient populations and removing barriers to accessing innovative drugs, devices, and therapies. In the case of ESRD, building partnerships with community-based organizations to develop targeted interventions and earlier identification of CKD has the potential to prevent patients of all socioeconomic backgrounds from progressing to ESRD. Kidney care stakeholders are often best positioned to understand the needs of their patients and should leverage this knowledge to develop an actionable policy and advocacy strategy prioritizing the clinical and non-clinical needs of marginalized populations. While the comment window for the ESRD PPS proposed rule closes on August 31, this administration has stated its priority to address gaps in health equity and will likely seek additional policy changes in future rulemaking.
To learn more about the evolving kidney care space and how Avalere can help your business drive access and continuity of care in this dynamic time, connect with us.
Methodology
Avalere identified a cohort of Medicare FFS beneficiaries with ESRD in 2019 using the 100% file of Medicare FFS Parts A and B data, accessed via a research-focused data use agreement with the CMS. Inclusion criteria required 6 months of FFS enrollment and no enrollment in a Medicare Advantage plan in 2019. Transplant was indicated by a claim with Medicare Severity-Diagnosis Related Group (MS-DRG) 008 (simultaneous pancreas-kidney transplant) or MS-DRG 652 (kidney transplant) in 2019. Dialysis type was identified using a combination of type of bill and condition code, and home dialysis and center dialysis were not exclusive. Home dialysis was type of bill 072X with condition code 74 (indicates a patient who received dialysis services at home) or condition code 76 (indicates a patient who dialyzed at home but received back-up dialysis in a facility). Center dialysis was type of bill 072X with condition code 71 (staff-administered, in-center) or condition code 72 (self-administered, in-center). Race was identified using the Research Triangle Institute algorithm variable, and dual-eligible status includes both full and partial duals. The codes associated with KDE billing are Healthcare Common Procedure Coding System code G0420 (face-to-face educational services related to the care of chronic kidney disease; individual, per session, per one hour) and G0421 (face-to-face educational services related to the care of chronic kidney disease; group, per session, per 1 hour).




