COVID-19 Pandemic’s Considerable Impact on Skilled Nursing Facilities
Summary
The roll-out of the Patient-Driven Payment Model (PDPM) in October 2019 followed quickly by the COVID-19 pandemic presents challenges to understanding the extent to which increases in payment to skilled nursing facilities (SNFs) are due to the changes in the payment system versus changes in the patient populations served during the COVID-19 pandemic. Given the confounding effects of the pandemic and the new payment system, it is important to collect more data before evaluating the transition to the PDPM.Fiscal year (FY) 2020 was the first year of the new PDPM that the Centers for Medicare & Medicaid Services (CMS) developed for skilled nursing facilities. The CMS designed PDPM to be budget neutral relative to payments under the previous Resource Utilization Groups Version IV (RUG-IV) payment system. To maintain budget neutrality, any observed increases in payment under PDPM in FY 2020 are subject to a downward adjustment in future rates.
In its assessment of budget neutrality, the CMS estimated FY 2020 RUG-IV payments to be 5.3% higher than FY 2020 PDPM payments. After removing patients with a COVID-19 diagnosis on a SNF claim, the CMS found that the difference was 5.0%, attributing the 0.3% difference to increased spending to treat COVID-19 patients.
Avalere conducted an analysis to evaluate the comprehensive impact of the COVID-19 pandemic on SNF patients. Avalere used the Minimum Data Set (MDS) to analyze the percentage of patients with a respiratory diagnosis treated in SNFs in FY 2019 versus FY 2020. Avalere’s analyses also examined changes in patient case-mix by month to determine how COVID-19 may have impacted payments for SNF care over the course of the pandemic. This month-by-month analysis also allows for an understanding of how government-mandated changes to patient management and SNF operations may have affected Medicare payments for SNF care for COVID-19 and non-COVID-19 SNF patients.
Respiratory Diagnoses Were Significantly Higher in FY 2020
Though March 2020 marked the start of the COVID-19 pandemic in terms of the larger impact on the healthcare system, Avalere’s analysis of MDS assessment items for respiratory diagnoses (MDS Items I6200 and I6300) found a higher proportion of patients with respiratory diagnoses throughout FY 2020 relative to FY 2018 and FY 2019.
Guidance from the CMS on COVID-19 diagnosis coding was not available to SNFs until March 2020,1 but Figure 1 illustrates that respiratory diagnoses in SNFs were significantly higher in all of FY 2020 compared to prior years. While several factors may contribute to the higher rates of respiratory illness, it is conceivable that this sharp increase was driven in part by COVID-19 cases before the CMS instituted a formal COVID-19 diagnosis code and by undiagnosed cases throughout the year.
This finding suggests that the CMS’s claims-based approach using the COVID-19 diagnosis code may not have adequately captured the COVID-19 case volumes over the course of the pandemic.
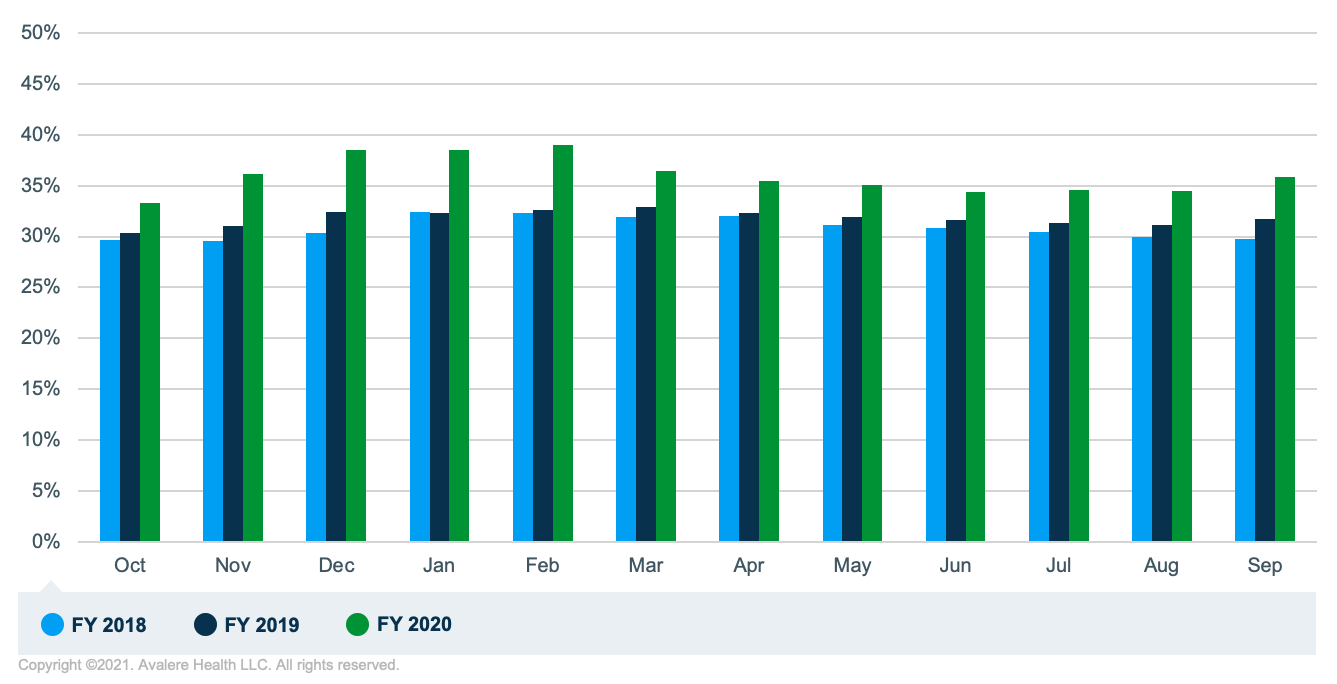
Avalere analysis of 2018–2020 MDS assessment data; MDS item I6200: Asthma, Chronic Obstructive Pulmonary Disease (COPD), or Chronic Lung Disease and MDS Item I6300: Respiratory Failure.
In addition to looking at the respiratory diagnosis items on MDS, Avalere also examined the ICD-10 diagnosis coding on MDS assessments and found that 10.3% of patients treated in SNFs had a diagnosis for COVID-19 over the course of FY 2020, with the highest number of cases occurring in April and May 2020.
Case-Mix Indices Increased for Non-COVID-19 SNF Patients
Avalere also examined changes in the acuity of beneficiaries treated in SNFs over the course of the pandemic. Under PDPM, the CMS bases payments to SNFs on 5 components of skilled care: nursing, speech-language pathology (SLP), occupational therapy (OT), physical therapy (PT), and non-therapy ancillaries (NTA).2 Each patient is classified for each of the case-mix adjusted components and the CMS multiplies the individual payment rates for the relevant components by a case-mix index (CMI). Each care component has its own CMI, which is designed to account for the patients’ acuity level. To determine the total payment for a given patient, the CMS sums the CMI-adjusted rates for the relevant components to arrive at the total payment level.
To look at how patient acuity levels changed as a result of COVID-19, Avalere analyzed changes in the CMIs across the 5 components of SNF care for patients with and without a COVID-19 diagnosis in both urban and rural settings. While there were was no change in the CMI for OT, PT, or NTA, the findings indicate that the speech-language pathology and nursing CMIs increased in April 2020 for COVID-19 and non-COVID-19 patients, and the CMIs remained high for the rest of FY 2020 relative to the pre-pandemic period (Figure 2). For example, the average nursing CMI in urban settings during the pandemic (March 2020-September 2020) for non-COVID-patients was 1.67 compared to 1.57 for the FY 2020 months prior to the pandemic (October 2019-February 2020).3
The increase in CMI for non-COVID-19 patients suggests that the pandemic’s effects extended to the broader SNF population, not just those with a COVID-19 diagnosis. The case-mix increases for patients without a COVID-19 diagnosis may reflect the increase in the acuity level of the beneficiary population treated in SNFs that resulted from the significant decline in post-surgical patient volumes, as elective surgeries were postponed due to the pandemic. Post-surgical patients are typically less complex relative to medical patients, so removing these cases could result in higher CMIs.

*Note that although October is included in this graph, assessments protocol was not the same as the rest of FY 2020. As October was the first month of FY 2020 and the PDPM, all residents were given an assessment, which is not standard procedure for the rest of FY 2020.
In addition to higher case-mix, the total number of total patients treated in SNFs was 14% lower at the end of FY 2020 compared to the beginning of the year, with the biggest drop in the census occurring between March and April of 2020 and continuing for remainder of the year.
Discussion
The COVID-19 pandemic has had a significant impact on SNFs. The decrease in total volume and the change in characteristics of the patient population, as demonstrated in the change in respiratory diagnosis and case-mix, suggest an impact broader than those with a claim diagnosis for COVID-19. The roll-out of the PDPM in October 2019 followed quickly by the COVID-19 pandemic presents challenges to understanding the extent to which unanticipated increases in payment to SNFs are due to the changes in the payment system versus changes in the patient populations served in SNFs during the COVID-19 pandemic. Given the confounding effects of the pandemic and the new payment system, it is important to collect more data before evaluating the transition to the PDPM.
Methodology
Avalere used the MDS Assessments to calculate total assessment volume for each month in FY 2019 and FY 2020 and the number of patients with and without a COVID-19 diagnosis or respiratory diagnosis. Assessments with B97.29 coding before April 1, 2020, and U07.1 for April 1 and onward in I0020B or any position of I8000 were analyzed for COVID-19 diagnoses. MDS items I6200: Asthma, Chronic Obstructive Pulmonary Disease (COPD), or Chronic Lung Disease and I6300: Respiratory Failure were examined as respiratory diagnosis over this period. The average CMI was calculated for each of the 5 components of CMI (nursing, NTA, PT, OT, SLP) for all patients and for those with and without a COVID-19 diagnosis.
Funding for this research was provided by the American Health Care Association. Avalere Health retained full editorial control.
To learn more about our work, connect with us.
Notes
- Prior to April 1, 2020, SNFs were instructed to code B97.29 for COVID-19 cases. Starting April 1, 2020, and onward, SNFs were instructed to use the code U07.1 (COVID-19).
- The NTA component is a score reflecting the medical complexity of each SNF patient. The score is calculated as a weighted count of 50 comorbidities and services.
- Averages are for SNFs in urban settings. In rural SNFs, the average post-pandemic nursing CMI for non-COVID-19 patients was 1.60 compared to 1.52 for the FY 2020 months prior to the pandemic.




