High-Intensity Prostate Cancer Costs Consistently Below OCM Benchmark
Summary
An Avalere analysis found differences in the performance of low- and high-intensity prostate cancer episodes in the Oncology Care Model (OCM). High-intensity prostate cancer episode expenditures were consistently below the benchmark price while low-intensity episode expenditures were similar to the benchmark price. This finding is likely driven by the Centers for Medicare & Medicaid Services (CMS) methodology used to calculate benchmark prices but may also indicate participant success in controlling costs for these episodes.The OCM is a voluntary, episode-based oncology-focused payment model from the CMS that aims to improve care coordination and reduce costs for Medicare fee-for-service (FFS) beneficiaries. The model evaluates the total cost of care for 6-month episodes initiated by chemotherapy treatments that are attributed to oncology practices participating in the model. Starting in July 2016, in each performance period (PP), the CMS has measured practice performance based on total episode expenditures relative to a benchmark price. The OCM prediction model is used to calculate the episode benchmark price based on historical spending that is projected forward using a common trend factor. Practice performance and practice elected risk track determine whether the practice earns a performance-based payment or owes a recoupment for the period.
Prostate cancer is 1 of the most common cancer types included in the OCM, and it accounts for nearly 11% of OCM episodes. Beginning in year 2 of the OCM, the CMS Innovation Center (Innovation Center) introduced risk stratification in the OCM prediction model to distinguish low-intensity versus high-intensity prostate cancer based on treatment utilized during the 6-month episode. Their categories are defined as follows.
- High-intensity prostate cancer: episodes with chemotherapy with or without androgen deprivation or anti-androgen therapy
- Low-intensity prostate cancer: episodes with androgen deprivation or anti-androgen therapy without chemotherapy
The CMS defines chemotherapy as any product on the “Oncology Care Models Initiating Therapies List.” They include the following drugs as androgen deprivation and anti-androgen therapies: bicalutamide, degarelix, flutamide, goserelin, histrelin, leuprolide, nilutamide, triptorelin.
High-intensity prostate cancer episodes may have a greater influence on OCM practice performance relative to low-intensity prostate cancer episodes because they account for a higher share of total episode spending.
- High-intensity prostate cancer accounts for 3.5% of OCM episodes and 4.5% of total OCM episode spending
- Low-intensity prostate cancer accounts for about 7% of OCM episodes, but only 2.5% of total OCM episode spending
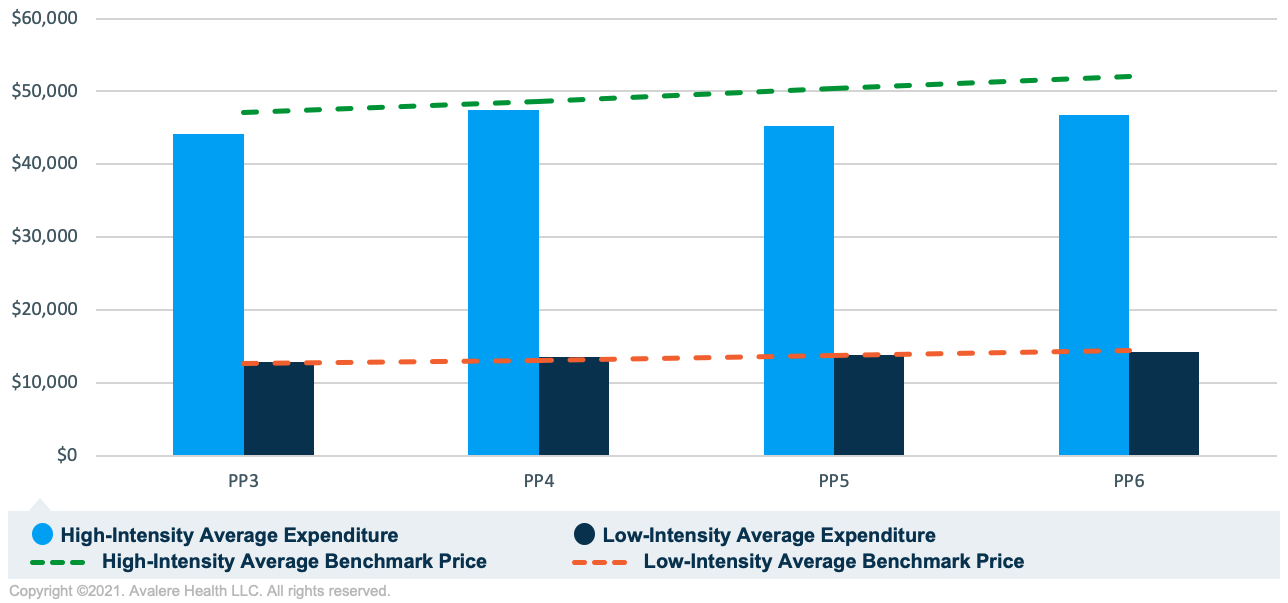
Avalere replicated the OCM program methodology and prediction model to calculate episode expenditures and benchmark prices. To compare episode performance between high- and low-intensity prostate cancer episodes, Avalere calculated the average episode expenditures and benchmark prices in PP3–PP6.
As shown in Figure 1, the average episode expenditures are consistently below the benchmark price for high-intensity prostate cancer episodes, an indication of strong performance among these episodes. The benchmark price increased 11% while average expenditures increased 6% from PP3–PP6. Avalere analyzed a subset of 20 OCM practices and found that 18 of these practices consistently had actual expenditures below the benchmark price in high-intensity prostate cancer, regardless of overall OCM performance. These findings may indicate that the OCM prediction model is overpredicting high-intensity prostate cancer benchmark prices or that practices are effectively controlling costs in this tumor type.
Low-intensity prostate cancer episode costs are much lower than high-intensity cancer episode costs given treatment differences between the groups. Many of the androgen deprivation and anti-androgen therapies used as treatment for this cancer type have generic drugs available and, therefore, drug spending is low among low-intensity prostate cancer episodes relative to high-intensity prostate cancer. As shown in Figure 1, average expenditures are nearly equal to the benchmark price in PP3–PP6, indicating that the OCM prediction model is more accurate for these episodes or that practices have been relatively successful in controlling costs in this tumor type.
Implications
As stakeholders await the Innovation Center’s announcement on the future of the OCM, which is set to end in June 2022, and its potential successor, the Oncology Care First (OCF) model, the lessons learned from the OCM might be best considered in the context of informing future models. This analysis reinforces the heterogeneity across and within cancer types in a model as complex as OCM. As discussed in the OCF request for information released November 2019, the Innovation Center suggested a tumor-specific trend factor and tumor-specific novel therapy adjustment. Implementing these changes may better align tumor-specific benchmark pricing with actual episode expenditures at the tumor level. The results of this analysis support additional model refinements, which may improve the prediction model. Previous Avalere analysis also identified bias in the OCM prediction model with respect to lung cancer. The model may not be appropriately accounting for advancements in treatment over time.
As the Innovation Center updates and introduces new models, it may face challenges related to design and participation as the healthcare industry continues to adapt to and recover from the COVID-19 pandemic. The disruptions in care will introduce new challenges to benchmarking and risk adjustment, particularly in oncology where delays in accessing care during the pandemic have led to more later stage cancer at the time of diagnosis. Ensuring an accurate risk adjustment and benchmarking methodology will be critical as the Innovation Center continues to encourage broad participation in value-based models.
To receive Avalere updates, connect with us.
Methodology
Avalere performed this analysis using Medicare Part A/B FFS claims and Part D prescription drug event data under a CMS research data use agreement. Avalere replicated the OCM program methodology developed by the CMS, including the attribution of episodes to practices, the assignment of cancer type, and the calculation of benchmark prices. Benchmark prices are calculated based on the CMS prediction model, which estimates episode costs based on key factors such as tumor type, beneficiary demographics and comorbidities, and utilization of certain services. Participants were identified in the claims data through tax identification numbers (TIN) reported on Part B claims. Avalere identified 174 practices that were ever enrolled in the OCM through TIN mapping and general research of oncology practices. This analysis includes practices active in the OCM as of July 2, 2021. The baseline period includes episodes initiated between January 1, 2012, and December 31, 2014, and the intervention period used for this analysis includes episodes initiated between July 2, 2017, and July 1, 2019 (PP3–PP6).







