MedPAC Proposes Replacement for MA Star Ratings Program
Summary
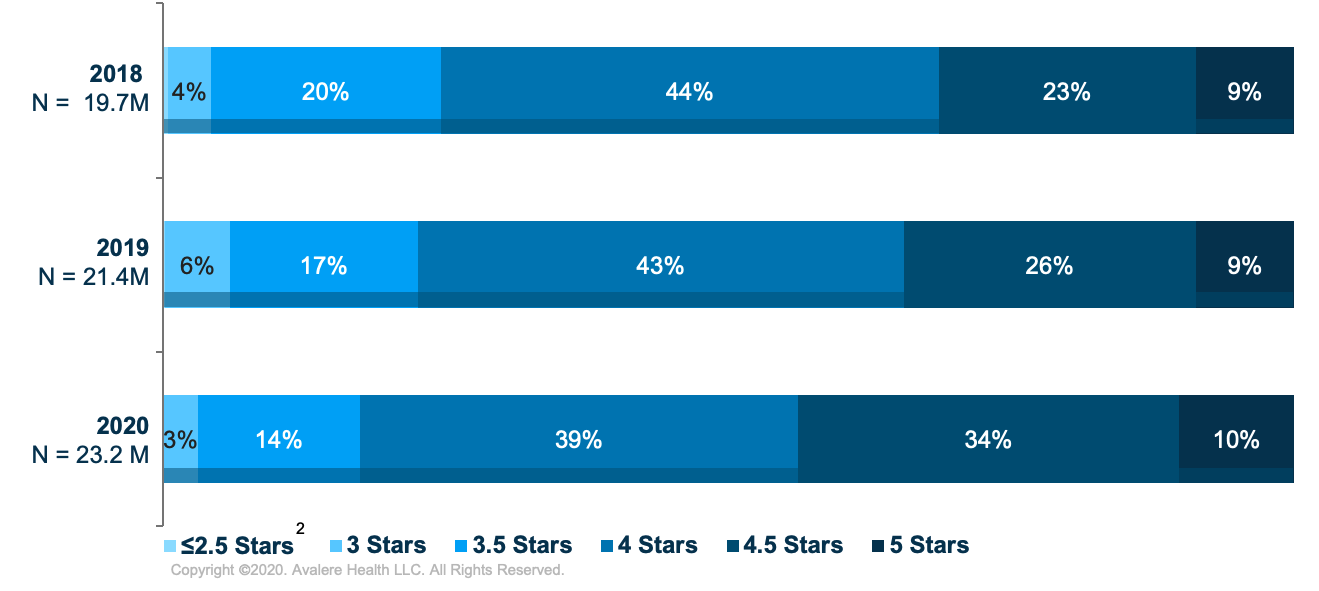
Under the Medicare Advantage (MA) Star Ratings Program, plans with 4-stars or more receive the greatest benefit from the Quality Bonus Program (QBP) in the form of higher benchmarks and bonus payments.The proportion of the MA market with 4 or more stars has grown in recent years. Avalere analyzed the current distribution of MA enrollees by star rating and found that 83% of enrollees are in plans rated 4 stars or more in 2020, a 12-percentage-point increase since 2018 (Figure 1). The Centers for Medicare & Medicaid Services (CMS) recently finalized several changes to the Star Ratings program that could impact plan ratings in the coming years. In addition to these near-term changes, broader fundamental changes to the program are also being considered.
Recent Significant CMS Updates to MA Star Ratings
On May 22, the CMS released the CY 2021 Medicare Advantage and Part D Final Rule. The final rule implements many MA proposals, including the following changes to the Star Rating measure system:
- Increase Weight of Patient Experience/Complaints and Access Measures: The CMS altered the relative importance of certain “patient experience” measures compared to other clinical and outcome measures when calculating MA contracts’ overall star rating. These weighting changes are set to be implemented in the 2021 measurement year, and the CMS indicated that the agency may increase the weighting of these measures even further in future rulemaking.
- Increase Stability of Star Rating Cut Points: The CMS revised its methodology for calculating star rating cut points, which will have the effect of shifting cut points upward and, therefore, overall star ratings and payments to plans downward. This change is set to be implemented in the 2022 measurement year.
In addition to the final rule, the CMS finalized a set of temporary COVID-19 flexibilities in an Interim Final Rule (IFR). The IFR suspends reporting requirements for Star Ratings in 2020, allowing the CMS to continue to use their 2020 scores. Notably, a suspension in MA Star Ratings data could impact the market for several years as measurement data is collected 2 years in advance of Star Ratings being released.
These changes will affect plans’ overall ratings, benefit design decisions, and payment for 2021 Star Ratings and beyond. Further, ongoing concerns about data collection and data reliability due to the continued effects of COVID-19 could drive the CMS to make additional modifications like the IFR in future years.
Looking Forward: MedPAC Proposed Replacement for MA QBP
In its June report, the Medicare Payment Advisory Commission (MedPAC) recommended overhauling the current MA QBP with a new value incentive program (MA-VIP). MedPAC has continually raised concerns about the QBP, highlighting, among other issues, that it is the only Medicare ”pay for performance” program that provides only additional payments to participants, whereas most other programs are budget neutral or penalty-driven.
MedPAC’s proposed MA-VIP includes the following changes:
- Reduce the total number of measures and focus on population-based and patient experience measures
- Introduce peer grouping to compare similar plans to account for social risk factors
- Require that payments to MA plans link to quality and do not increase overall Medicare spending
- Evaluate measure performance and adjust payment at the local level
- Establish pre-determined performance targets for individual measures
Implementation of the MA-VIP system would affect all MA plans. Plans with 4 stars or higher that receive an increase in their benchmarks could be at risk for losing part or all of their payment “bonus.” Changes to plan’s star rating performance not only impacts plan payment but also potentially impacts plan enrollment, premiums, and supplemental benefits. The magnitude of these changes will depend on the impact of shifting toward a budget-neutral system and how a plan’s individual circumstances adapt to the individual components of MedPAC’s recommendation.
While the proposed change for budget-neutral quality bonuses could negatively impact most plans, the remaining recommendations (e.g., reducing the number of measures) could impact individual plans differently depending on a host of factors, including:
- The proportion of a plan’s enrollment of low-income individuals and individuals with disability
- Quality differences among plans within a local market
- A plan’s performance on population health measures compared to disease-specific or process measures
Importantly, some of MedPAC’s proposals could potentially be enacted by the CMS through annual rulemaking, and others would require congressional action. For instance, legislation would likely be required for any action that changes payment to plans as a result of a plan’s star rating. Congress has recently acted in this area, as evident in a 2018 law, limiting payment to plans that merged 2 contracts. Conversely, the CMS has wide discretion to make changes in how MA plans’ star ratings are calculated and what types of quality measures should be used in the system.
Stakeholders can anticipate that these proposed changes may move separately and can develop customized engagement strategies with the CMS and Congress around certain components.
To receive Avalere updates, connect with us.







