Medication Adherence Disparities Linked to Race, Socioeconomic Factors
Summary
An Avalere analysis finds that a smaller share of Black and Hispanic Medicare beneficiaries and beneficiaries in lower socioeconomic quartiles have sufficient adherence for commonly used medications. The analysis also shows greater disparities in Medicare plans rated 3 stars or fewer.Under the Medicare Star Ratings program, Medicare Advantage (MA) and Part D plans are rated across a variety of measures to evaluate plan quality. Individual measure and overall ratings range from 1 star (lowest quality) to 5 stars (highest quality). The Star Ratings may guide beneficiaries who are comparing plans on Medicare Plan Finder. Additionally, MA plans are incented to achieve higher quality ratings, as plans that have an overall rating of at least 4 stars receive bonus payments that can be used to cover additional benefits for enrollees.
Reports released by the Centers for Medicare & Medicaid Services’ (CMS) Office of Minority Health have shown that prescribing, beneficiary medication use, and plan performance on clinical care and patient experience measures vary based on beneficiary demographic factors. While the reports highlight disparities in these areas, they provide limited insight into how medication adherence levels may differ across Part D plans and by plan quality rating.
To further investigate these findings, Avalere analyzed Medicare Advantage prescription drug plan (MA-PD) and standalone prescription drug plan (PDP) performance on medication adherence measures for 3 therapeutic areas: diabetes, hypertension, and cholesterol. The analysis examined whether a plan’s overall star rating was correlated with adherence for these disease states and if this relationship varied by beneficiary group.
Specifically, Avalere analyzed 2020 performance data for 3 measures developed by the Pharmacy Quality Alliance related to medication adherence: Medication Adherence for Diabetes Medication (does not include insulin medications), Medication Adherence for Hypertension (renin-angiotensin-system [RAS] antagonists), and Medication Adherence for Cholesterol (statins). Adherence for these measures is based on the proportion of days covered (PDC). According to the Pharmacy Quality Alliance, a PDC of at least 80% is recognized as the threshold above which a beneficiary is reasonably likely to receive the most clinical benefit from a medication. Avalere refers to achievement of a PDC score of 80% or more as “sufficient adherence” throughout this piece.
Across both MA-PDs and PDPs, Avalere assessed the percentage of beneficiaries reaching a PDC of ≥80% (i.e., percentage of beneficiaries with “sufficient adherence”) for the 3 measures and stratified the results by race, socioeconomic status (SES), low-income subsidy (LIS) status, and plan type. Avalere leveraged an Agency for Healthcare Research and Quality report for categorizing Medicare beneficiaries’ SES by residential ZIP code, which includes a variety of factors collected through the census to determine SES, such as employment, income, education, and housing.
Findings
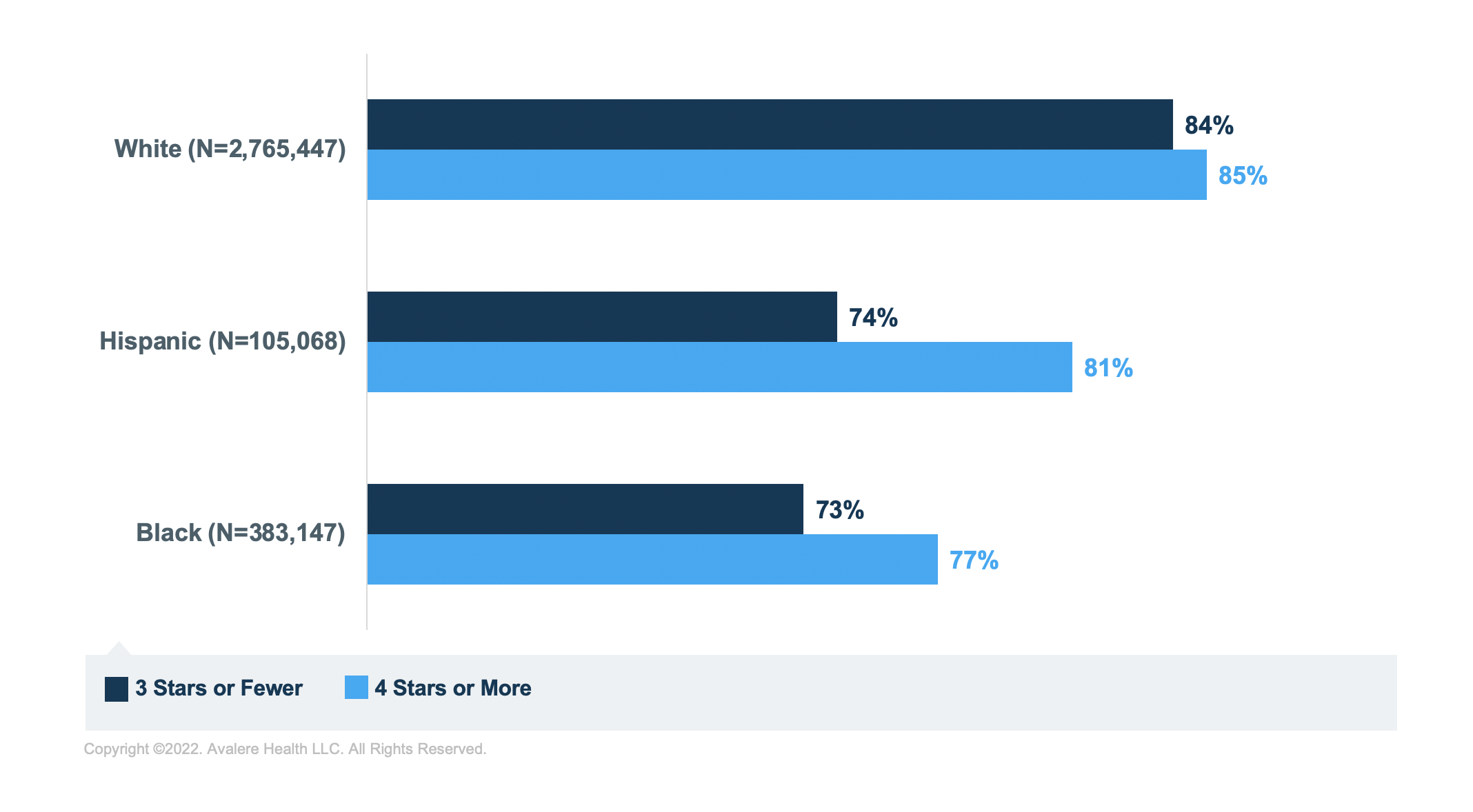
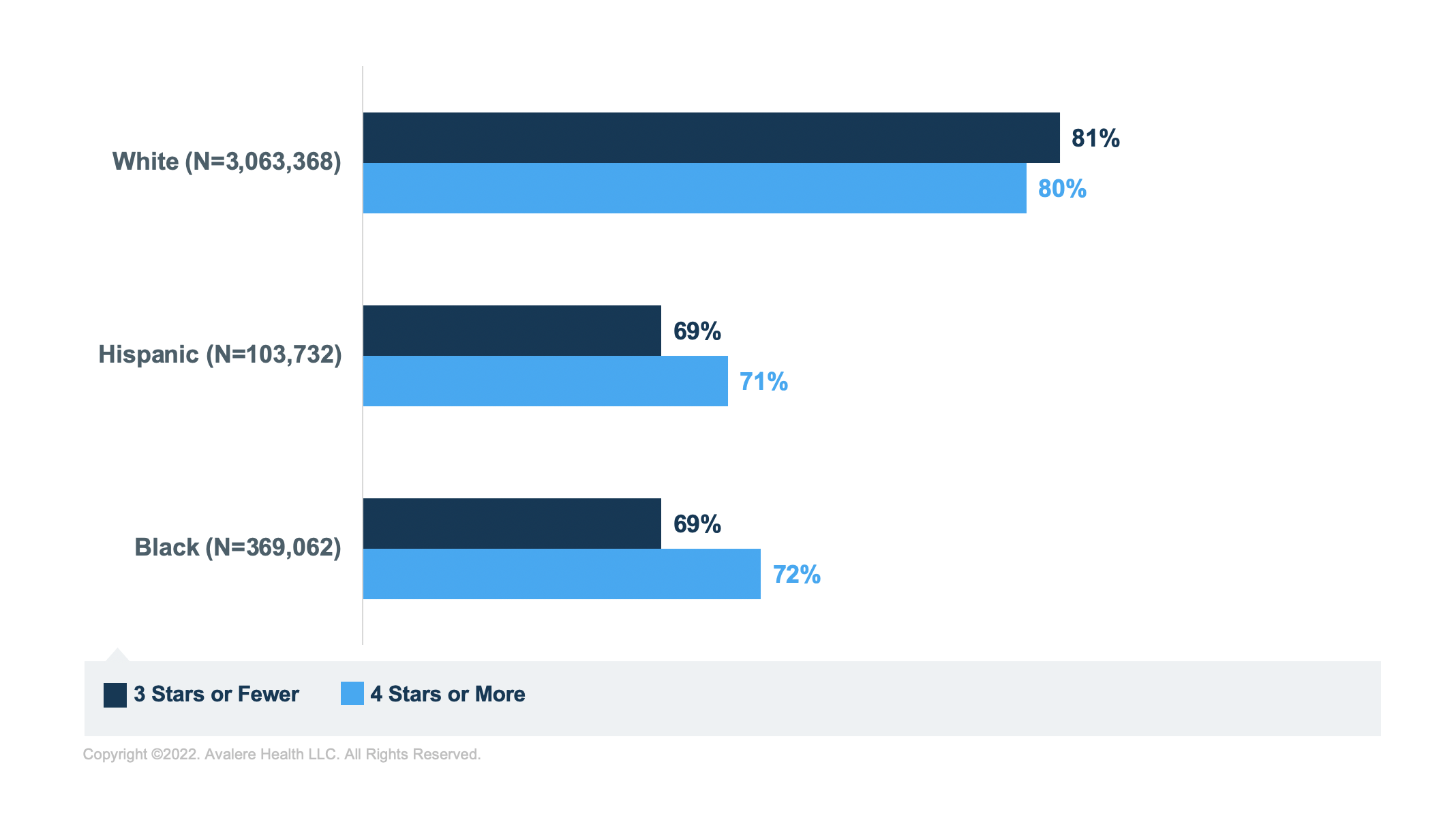
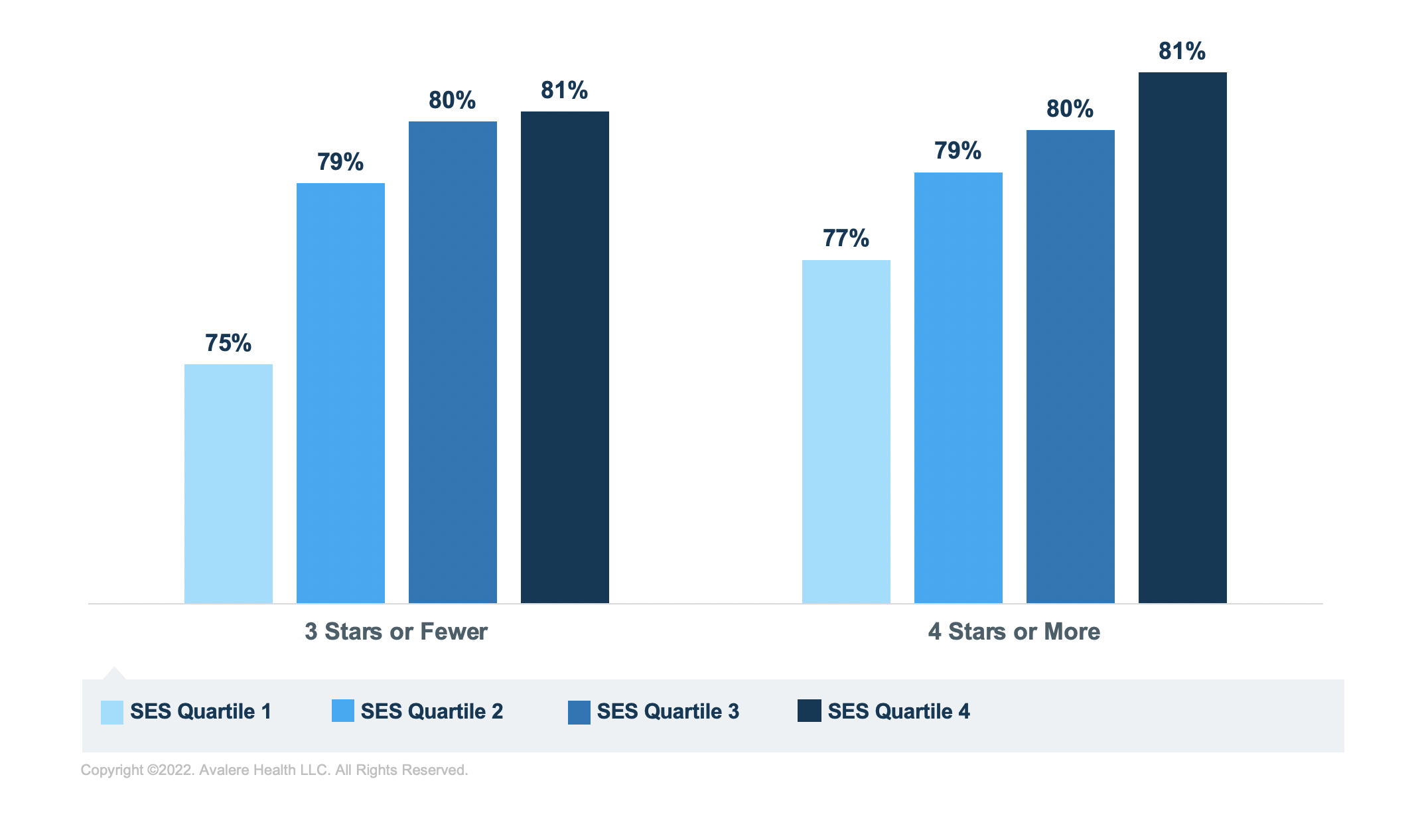
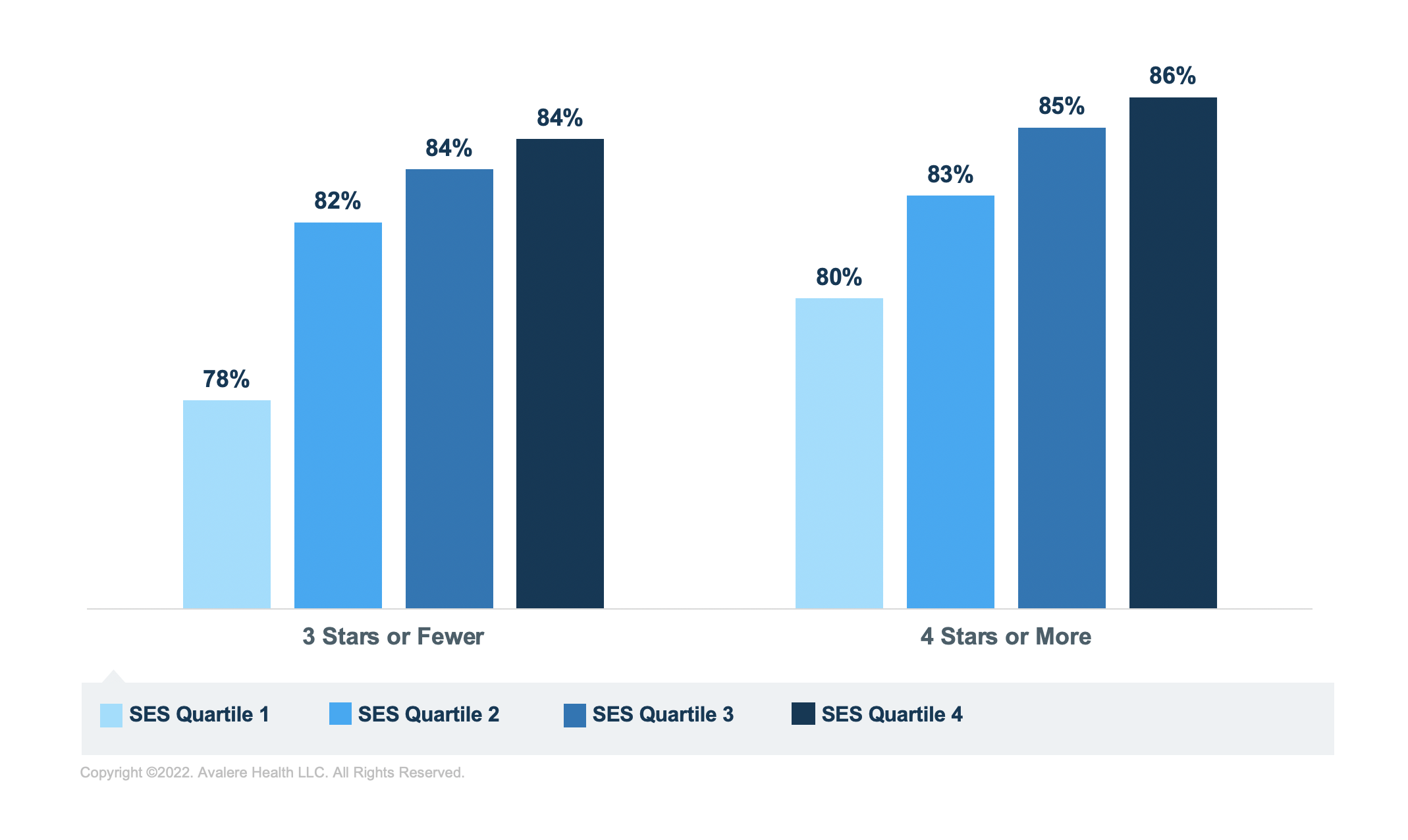
Avalere’s analysis finds that across the disease states analyzed, a smaller proportion of Hispanic and Black beneficiaries had sufficient adherence when compared to White beneficiaries. Additionally, a lower share of beneficiaries in the lowest SES quartile had sufficient adherence compared to beneficiaries in the highest SES quartile. These differences varied by plan type (i.e., PDP vs. MA-PD), LIS status, and plan star rating, but were directionally the same.
The graphic below depicts these disparities, showing the percentage point difference in the share of beneficiaries with sufficient adherence between groups. Darker shades of colors indicate greater disparities in the share of beneficiaries with sufficient adherence between the groups being analyzed.
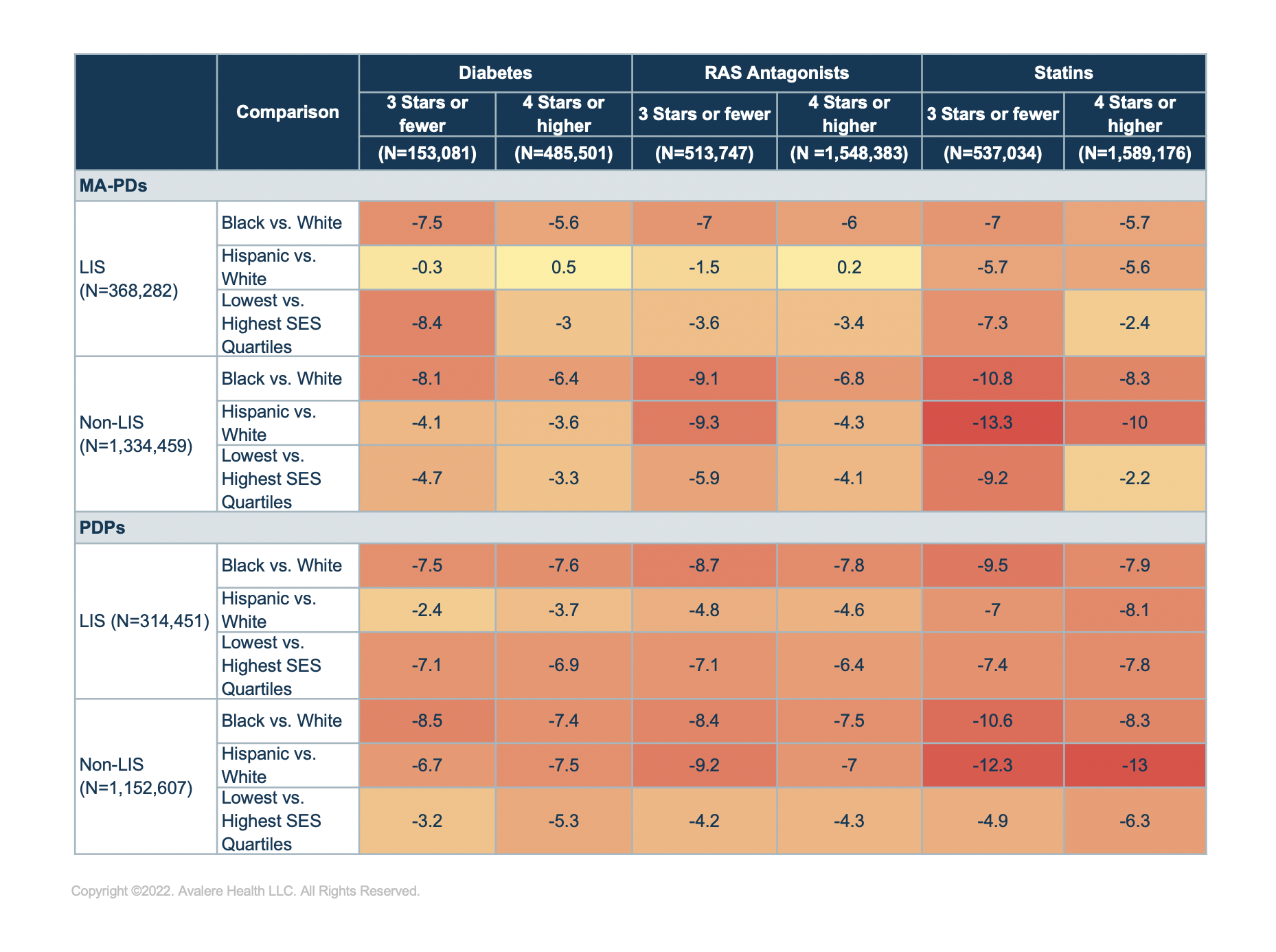
As shown in Figure 1, beneficiaries taking statins had the largest disparities in the share of enrollees with sufficient adherence across race/ethnicity comparisons. For instance, across non-LIS beneficiaries in MA-PDs rated 4 stars or higher, the share of Hispanic beneficiaries with sufficient adherence for statin medications was 10% lower compared to White beneficiaries. These disparities persisted but were smaller for beneficiaries taking RAS antagonists and diabetes medications (4.3% and 3.6%, respectively).
Additionally, racial and ethnic disparities in the share of enrollees with sufficient adherence for statin medications were greater for non-LIS beneficiaries than for LIS beneficiaries (Figure 1).
As illustrated in Figure 1 and in the charts below, disparities by race/ethnicity and SES were generally greatest among beneficiaries enrolled in lower-rated plans (plans with 3 stars or fewer) compared to higher-rated plans (plans with 4 or more stars). For example, among beneficiaries taking diabetes medications across all plan types, 71% of Black beneficiaries enrolled in plans rated 3 or fewer stars had sufficient adherence compared to 74% of Black beneficiaries in plans rated 4 stars or higher and 80% of White beneficiaries (Figure 2).
Among all beneficiaries, enrollees taking statins in plans rated 3 or fewer stars had the largest disparities when comparing SES quartiles, with only 74% of enrollees in the lowest SES quartile having sufficient adherence compared to 82% of enrollees in the highest SES quartile (Figure 3).
Looking Ahead
Findings from this analysis highlight disparities by race/ethnicity and SES in the share of beneficiaries with sufficient medication adherence, with greater disparities for enrollees in plans with 3 or fewer stars. As the CMS and other healthcare stakeholders continue to explore policies focused on advancing health equity, disparities in medication adherence and their relation to plan star ratings may be an area of further study and focus by the CMS.
In the 2023 Advance Notice released on February 2, the CMS considered several potential changes to the Star Ratings program, which would affect how the CMS measures and addresses disparities. For example, the CMS noted it is continuing to explore the possibility of risk adjusting the 3 medication adherence measures by beneficiary-level SES, such as LIS, dual-eligible status, and disability factors to adequately reflect differences in patient populations. The CMS is also seeking public input on multiple proposed measure concepts focused on identifying and reporting disparities, such as a health equity index that would summarize plan performance among enrollees with social risk factors across multiple measures.
Funding for research provided by the Pharmaceutical Research and Manufacturers of America (PhRMA). Avalere maintained full editorial control.
To receive Avalere updates, connect with us.
Methodology
Avalere used 2019 Medicare Part D Drug Event (PDE) data, accessed via a research-focused data use agreement (DUA) with the CMS to determine the medication adherence for 3 selected medication categories: diabetes, RAS antagonists, and statins.
Utilizing the exclusion and inclusion criteria of the targeted medications specified for each measure and the 2019 PDE, Avalere calculated each beneficiary’s PDC, which is the sum of the number of days a beneficiary was covered by at least 1 drug in the class based on the prescription fill date and days of supply divided by the number of days in the beneficiary’s treatment period. The treatment period is defined as the fill date for the first drug in the class to the end of the enrollment period, disenrollment, or death.
Avalere identified the 2019 Agency for Healthcare Research and Quality SES index from the Acxiom’s InfoBase Geo files to assign SES levels to beneficiaries based on the ZIP code where they reside. Beneficiaries are then grouped into 4 SES levels corresponding to the quartiles of the SES index specific for the Medicare fee-for-service population. Lastly, Avalere identified plans’ star ratings from 2020 plan ratings that are publicly available from the CMS website.
Per the DUA’s requirement, Avalere identified a random sample representing less than 20% of the total Part D population. Avalere did not include beneficiaries in the US territories and beneficiaries that were enrolled in the Limited Income Newly Eligible Transition Program were excluded from this analysis.