Identifying Payer and Provider Opportunities for Quality Measures Alignment
Summary
This past spring, Avalere and MITRE experts presented “Implementation of the Core Quality Measures Collaborative (CQMC) Core Measure Sets by Public Payers: Successes and Opportunities” at the Pharmacy Quality Alliance (PQA) annual meeting.Using Avalere Quality Measures Navigator® (QMN) as the source for measure data and MITRE’s Measure Alignment Aid, the research sought to systematically identify successes and opportunities in the development and implementation of the CQMC Core Sets by public payers, specifically the Centers for Medicare and Medicaid Services (CMS). Additionally, the analysis proposed recommendations to the CQMC as they work to update the core sets in this next phase of the Collaborative, the first update since their introduction in 2016.
The CQMC was established in 2015 and released 7 core measure sets (Core Sets) of quality measures intended to support greater quality improvement and reporting across the health system. The pediatric core set of measures was added in 2017 for a total of 8. The CQMC is spearheaded by CMS and America’s Health Insurance Plans– in partnership with the National Quality Forum. It includes 55 member organizations and is governed by a Steering Committee – comprised of experts from insurance providers, businesses, primary care and specialty societies, patient groups, measurement experts, and regional leaders.
Findings and Recommendations
CQMC Core Set
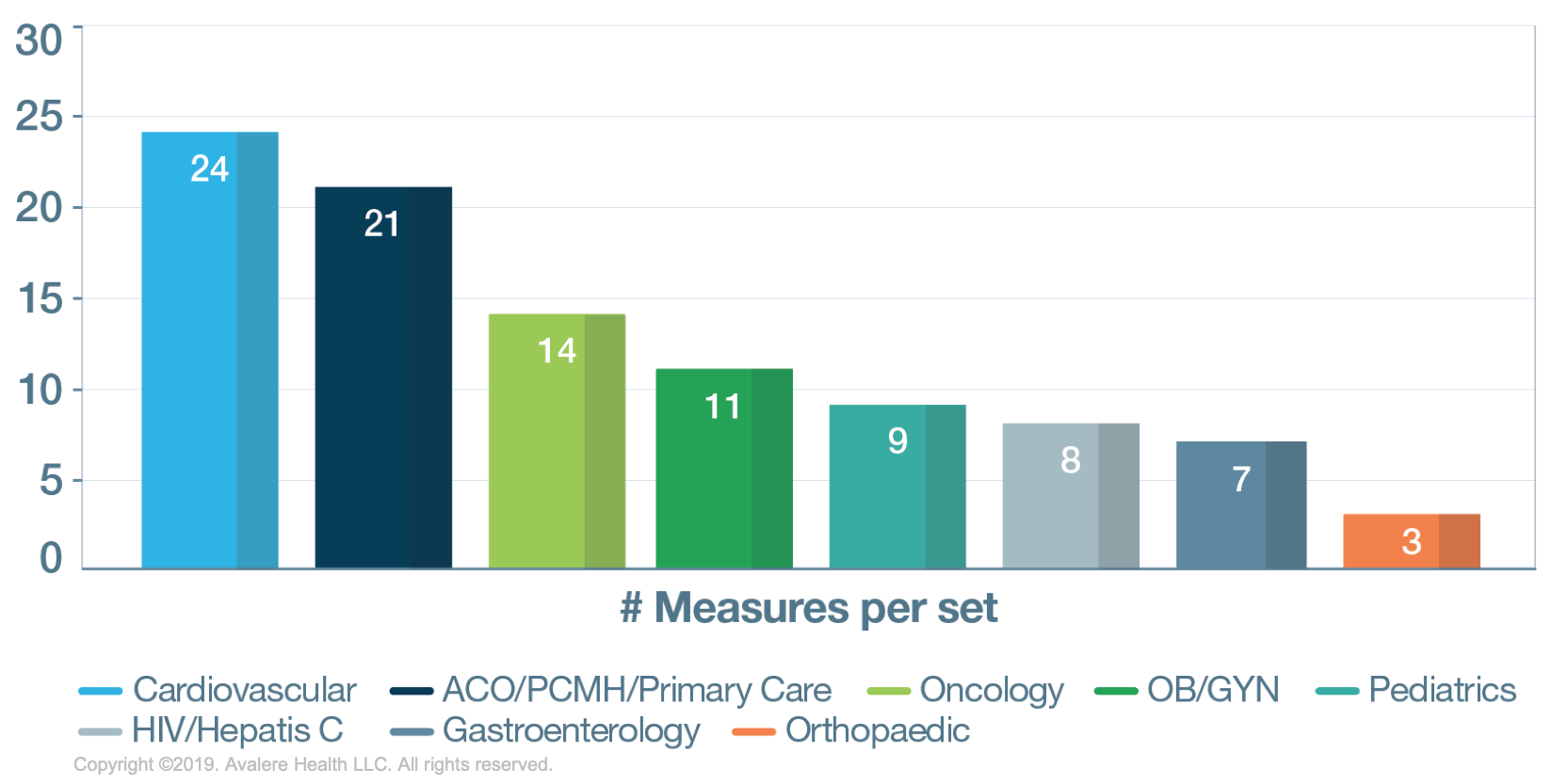
There are 90 unique CQMC measures included in 8 different core sets of varying size. The research found that the orthopedic core set is the smallest (n=3), potentially indicating a gap area since this is a high-cost and high-utilization area, particularly in the elderly population.
Given the high number of measures in this specialty area (>250), the CQMC could consider adding recently developed, high-value measures in the orthopedic core set, such as functional status assessment for total hip and knee replacement (Merit-based Incentive Payment System [MIPS] measures) and trauma measures.
If CQMC chooses to continue prioritizing measures using the current specialty-specific framework, the CQMC should consider aligning their sets with the specialty sets used in the MIPS program in addition to developing well-defined prioritization factors for the development of new core sets.
Measure Type
Approximately 4% of the 90 total measures are patient-reported outcomes (PROs). Given that patient-centered measurement is a key focus of the administration as part of the Meaningful Measures Initiative, the CQMC should identify recently developed PROs—particularly those that are condition specific—to add to the individual core sets. For example, the American Urological Association’s measure “Prostate Cancer: Patient Report of Urinary Function After Treatment” could be added to the Oncology Core Set, which currently includes zero PROs. The significant number of process measures should also be evaluated for continued value and impact.
National Quality Strategy Priority
Our analysis found that only 3% of CQMC measures focus on communication and care coordination. Additionally, 9% of these measures related to efficiency or cost reduction.
Should CQMC decide to take the “cross-cutting priorities” (i.e., specific goals or priorities that cut across care settings, conditions, or payment models) approach, they may need to address the lack of appropriate measures in areas like care coordination and cost and efficiency.
Use of CQMC Measures in 2019 CMS Programs, Based on Their Accountability Level
Sixty-two percent (56/90) of CQMC measures are included in MIPS, the CMS clinician-level quality program. The recent CMS focus on alignment and deduplication has reduced the inclusion of a single measure in multiple medical system level programs, evidenced in the smaller number of measures in each of the 8 hospital-focused programs. Although there are fewer measures specified at the managed-care level (n=26), those measures are more highly utilized across the 4 relevant programs.

It should be noted that 21% (19/90) of CQMC measures are not included in any CMS programs as of 2019, so they are not represented in this figure.
The CQMC should determine whether measures that are currently only targeted towards clinicians are readily usable by health plans or hospitals.
Data Sources
CQMC measures use a variety of data sources; this analysis, however, found that only 27% use electronic health data in their specifications. Of additional interest was the fact that 42% of the CQMC measures now use registry data. A report from AHIP noted that registries are a growing area of interest for health plans given that they may ease EHR data collection burden on individual providers.
The CQMC should explore additional measures that are e-specified for potential inclusion in the core sets to reduce the burden on clinicians. To address issues with comparability and data sharing across different insurers, the creation of standardized value sets should be considered to simplify data capture and encourage use of the core sets.
Additionally, the CQMC has an opportunity to encourage the continued adoption of registry-specified measures by the health plans and assess qualified clinical data registry measures for potential future inclusion in the core sets.
Three Key Takeaways
- As the CQMC looks to revamp the core sets, it is crucial to analyze the current sets holistically and look for areas for improvement and gaps. Unfortunately, there is currently no publicly available measure repository that contains all quality measures, including their use in quality programs, and only QMN—a subscription-based repository—combines measures from multiple sources in one place.
- There are multiple opportunities for continued alignment of the CQMC measures. For example, additional analysis conducted by the MITRE Corporation as part of the PQA poster presentation indicated that the 21% of CQMC measures not currently in use by CMS programs show ready opportunities for adaptation or outright adoption to improve comparability and fill gaps across federal payment programs. Given that the timeline to adopt measures into public and private payer programs can span multiple years and many organizations report to more than one quality program, stakeholders should expect for it to take years to align measures across programs. Despite the extended timeline, alignment will improve clarity and foster focus, organization, and consistency among existing measures used in federal, state, and private improvement efforts.
- A holistic, multi-stakeholder approach to maintaining the core sets, including frequent reviews and updates, will be critical to their successful uptake moving forward. This will require ongoing input and review from stakeholders, consistent standardization of templates across sets, and potential integration with the federal rule-making cycle and NQF endorsement process. The purview of the CQMC and its members should be expanded to include a designated responsibility for maintaining the CQMC measure sets and coordinating their implementation moving forward.
To learn more about how QMN can inform your business strategy, contact Daniel Day.
To receive Avalere updates, connect with us.