EOM Participation Likely Influenced by Prior OCM Experience
Summary
With EOM’s immediate downside risk, the model may appeal more to practices ready to implement care transformation activities and value-driven decision making.The Oncology Care Model (OCM) was a voluntary, 6-year, episode-based, oncology-focused payment model from Center for Medicare & Medicaid Innovation (CMMI). The model aimed to improve care coordination and reduce costs for Medicare Fee-for-Service (FFS) beneficiaries, and it evaluated total cost of care for 6-month episodes. The OCM concluded June 30, and its successor, the Enhancing Oncology Model (EOM), will begin July 1, 2023.
The EOM methodology design was informed by learnings from the OCM. The CMMI is making several key changes that will affect the number of included beneficiaries and maximize the opportunity for savings to Medicare. The EOM requires practices to immediately take on downside risk and reduces the monthly enhanced oncology services payment per beneficiary per month from $160 to $70, while requiring participants to implement additional redesign activities. Stakeholders are considering what these changes mean for participation in the EOM.
To better understand and predict EOM participation considering lessons learned from OCM, Avalere analyzed OCM performance within the context of practice type and ability to achieve a performance-based payment (PBP).
Findings
The majority of OCM episodes were attributed to community-based practices. About two-thirds of the 126 active OCM participants were community-based and accounted for over 80% of overall OCM episode volume. Based on the classifications above, 35% of community practices were considered “higher performing.”
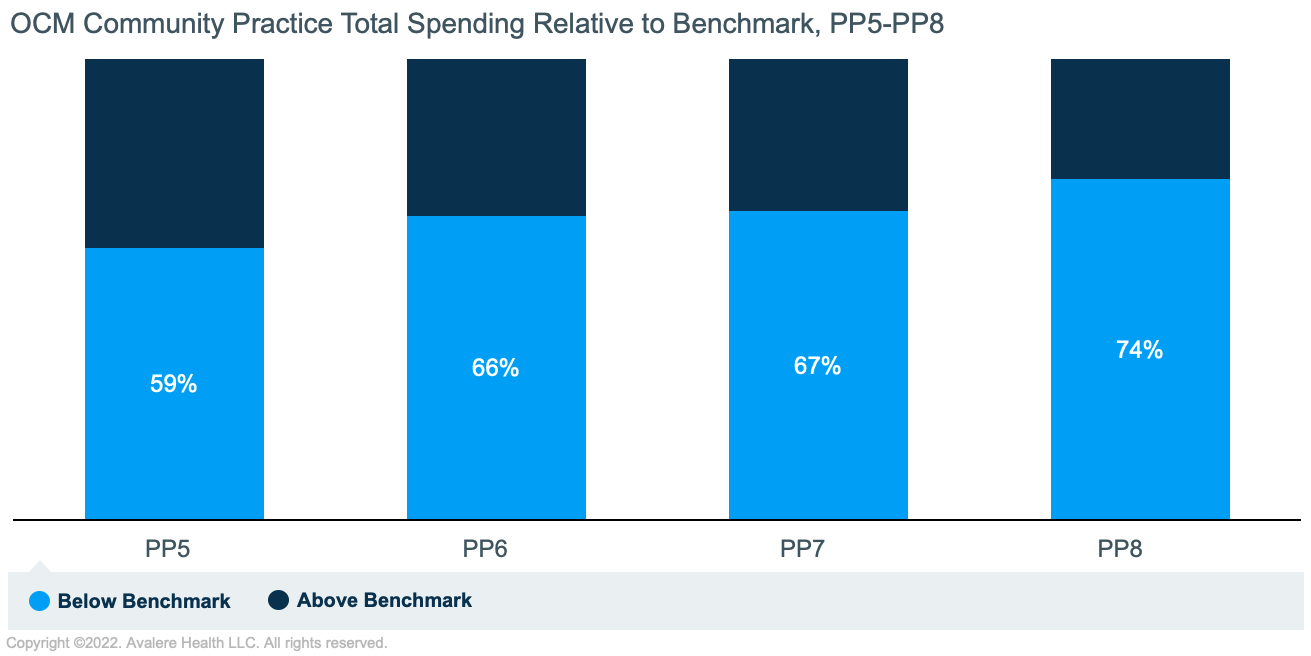
To examine elements of practice success in OCM, Avalere assessed practice performance among community-based practices for Performance Period (PP) 5 through PP8 (episodes initiated between July 2018 and June 2020 and ended by December 2020). Practices were classified into performance categories based on historic performance.
- Higher Performing: Earned 3–4 PBPs in PP5–PP8 in alternative two-sided risk
- Lower Performing: Earned at least 0–1 PBPs in PP5–PP8 in alternative two-sided risk
- Other: Earned 2 PBPs in PP5–PP8 in alternative two-sided risk
Community-based practice performance improved over time. Model savings are achieved when practice expenditures are below the benchmark amount defined by CMMI. From PP5 through PP8, the share of practices with total expenditures below the benchmark amount increased from 59% to 74% (Figure 1), which suggests that performance improved as participants became more familiar with the model. Given the pattern of improved performance over time, experienced OCM practices with demonstrated patterns of achieving PBPs may be positioned more favorably as they contemplate participation in the EOM. EOM participants who have not participated in an OCM or commercial oncology alternative payment model (APM) may experience a learning curve in the first one to two years of the model.
Smaller episode volume has been associated with OCM success. Using average episode volume per practice and PP as a measure of practice size, Avalere found that “higher performing” practices were 26% smaller than “lower performing” practices (Table 1). Smaller practices may benefit from smaller, more centralized decision-making and dissemination processes that allow them to implement organizational changes more quickly with greater impact on OCM performance.
Two community oncology practices contribute about 20% of OCM volume. To remove potential bias that these practices have on an assessment of average episode count, Avalere also assessed average episode count without these practices. When excluding the largest community oncology practices, “higher performing” practices were 45% smaller than “lower performing” practices.
| All Community Oncology Practices | Excluding Largest Community Oncology Practices | |||
|---|---|---|---|---|
| Higher Performing | Lower Performing | Higher Performing | Lower Performing | |
| Average Episode Count Community practices (n=80) |
217 | 294 | 120 | 219 |
Among the 80 community oncology practices, Avalere observed similar patterns related to average episode expenditure, tumor mix, and OCM methodological adjustment factors across practices (Figure 2).
- Avalere assessed the cost components that make up community oncology episodes’ total cost of care. On average, most costs in PP5–PP8 were attributed to Part B oncolytics followed by Part D oncolytics (Figure 2).
- Practices’ tumor mix was very similar across the 80 community oncology practices. The seven tumor types that will be included in the EOM accounted for nearly half of all OCM episodes in PP5–PP8 (Figure 2). Practices considering participation in EOM Risk Arrangement 2 should estimate whether their EOM episode volume will meet the threshold to achieve Qualified Professional (QP) status or partial QP status under the Medicaid and Children’s Health Insurance Program Reauthorization Act, which exempts them from Merit-based Incentive Payment System reporting and, for QP status, earns higher annual payment updates.
- To estimate the benchmark amount, the OCM methodology included three adjustment factors: the trend factor, novel therapy adjustment, and experience adjustor. These adjustments aimed to account for a practice’s historic efficiency and cost patterns. Avalere assessed variation across three adjustment factors by participant success category and found that the distribution of these values was very similar and did not drive the likelihood of success.
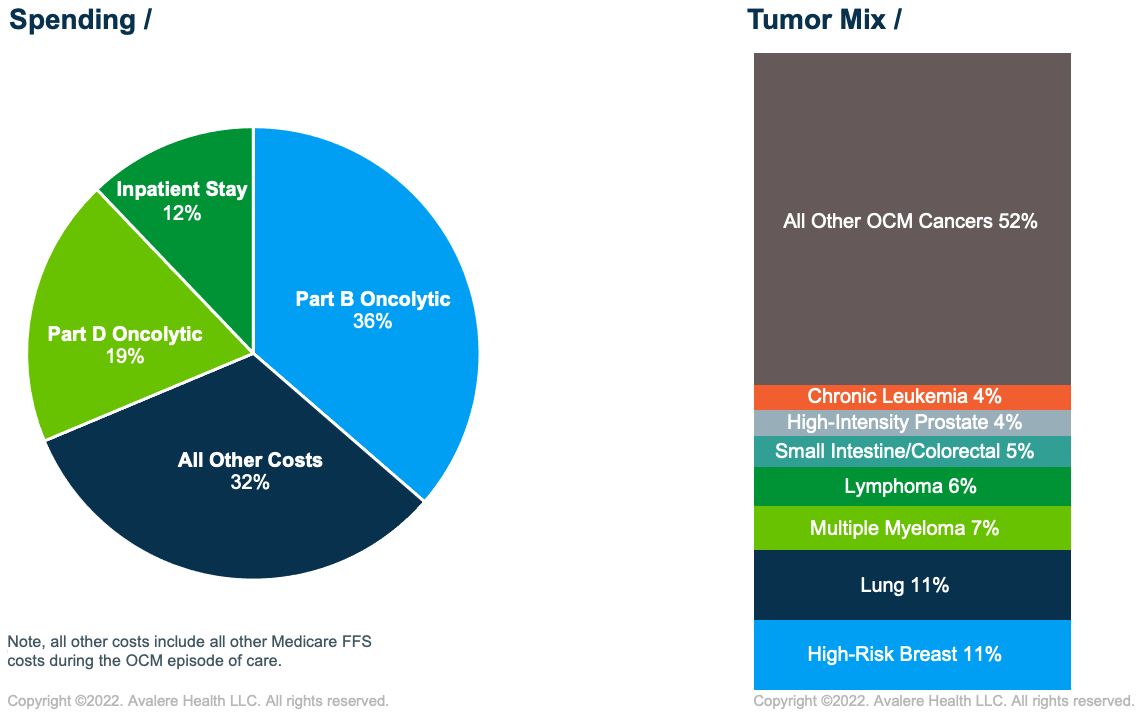
Note: all other costs include all other Medicare FFS costs during the OCM episode of care.
As community oncology practices further advance participation in APMs, they face challenges to implementing care redesign and taking on more downside risk in a primarily FFS environment. When deciding whether to participate in the EOM and other commercial models, practices must consider APM design in addition to established practice economics in a post-COVID-19 world. Although smaller practice size was associated with higher performance in the OCM, practices of all sizes may engage in the EOM. Characteristics of practices likely to participate in the EOM may include financially higher performing OCM participants, practices with network-level support navigating the model and implementing care transformation, and practices involved in commercial APMs.
What’s Next?
The time between the EOM request for application announcement on June 27, 2022, and the model commencement on July 1, 2023, offers an opportunity for stakeholders to understand the design, model the impact, and engage with CMMI to continue to shape the model. Avalere can help life sciences companies and other stakeholders assess how the EOM will impact practice performance and model-associated revenue streams.
Funding for this research was provided by the Community Oncology Alliance. Avalere maintained full editorial control.
Methodology
Avalere replicated CMMI’s OCM methodology using Medicare FFS Part A and B and Part D prescription drug claims data. Episodes were assigned to practices using a proprietary taxpayer identification number mapping algorithm; 124 of the 126 active OCM practices were identified for analysis. OCM practice type (i.e., community vs. hospital-based) was identified using a two-part approach. First, practices were classified according to the most frequent place of service (i.e., physician office for community and hospital outpatient for hospital-based) observed on the cancer-related evaluation and management visits billed during their attributed episodes. Second, a manual review was conducted to reclassify ten practices that were likely hospital-based but had varying billing patterns indicating a physician office place of service.
At the PP level, Avalere defined OCM success based on comparing practices’ actual spending relative to the benchmark amount (i.e., ability to earn a PBP or risk of owing recoupment). For each PP, practices were classified into one of four performance zones based on their distance to benchmark, defined as the ratio of actual spending to benchmark amount. The figure below shows the mapping between performance zone and the distance to benchmark value.
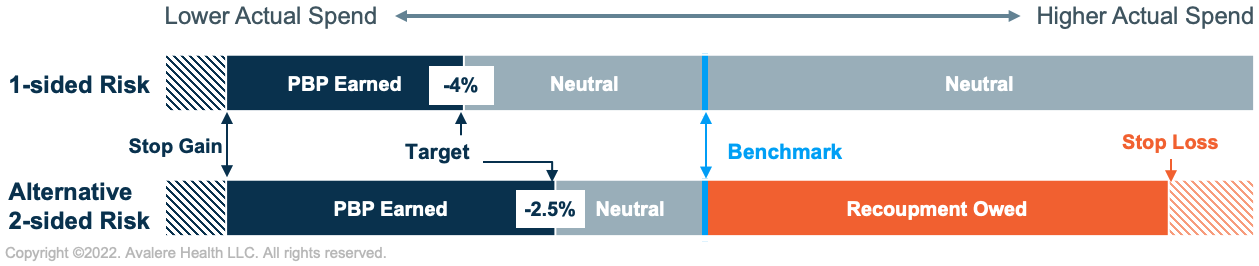
Since performance can vary for a given practice across the four PPs in the analysis, Avalere assessed the number of PPs from PP5 to PP8 for which a practice was estimated to have earned a PBP under an alternative two-sided risk arrangement (i.e., distance to benchmark was -2.5% and below). Practices estimated to have earned three or four PBPs were considered to be “higher performing” while practices estimated to have earned between zero and one PBPs were considered “lower performing.” Practices estimated to have earned two PBPs were categorized as “other.”
To keep up with the latest developments in oncology care models, connect with us.







