CMS Creates New Codes to Reimburse for Navigation Services
Summary
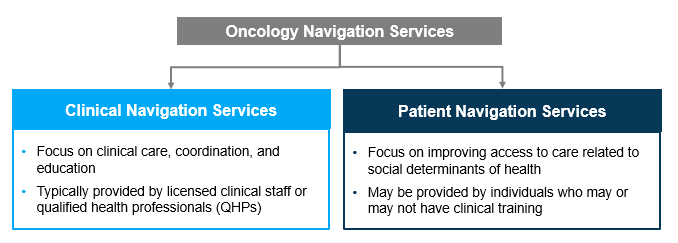
Newly developed HCPCS codes will support increased access to oncology navigation services, which have been shown to improve patient outcomes.Patients seeking cancer care may face financial (e.g., lack of insurance), cultural (e.g., language barriers), and systemic (e.g., uncoordinated care) barriers, which can delay access to treatment. Patient and clinical navigation services aim to address patient barriers to accessing timely care. These services include helping patients manage referrals and follow-ups, schedule appointments, and identify social support programs. According to the Oncology Navigation Standards of Professional Practice there are two categories of oncology navigation services provided to patients (Figure 1).
Figure 1: Types of Oncology Navigation Services
Oncology navigation programs are often funded through short-term grants provided by government agencies such as the Centers for Disease Control of Prevention or advocacy organizations such as the American Cancer Society. However, grants are time-limited, and oncology providers must find long-term, sustainable funding sources to maintain this infrastructure after funding subsides.
Before 2024, any codes available for general navigation services were limited to services provided by clinical staff and QHPs. However, non-clinical patient navigators offer services and resource connections, relieving clinical staff from tasks that would otherwise detract from direct patient care during appointments.
New CPT Codes Established to Address Gaps in Available Navigation Service Codes
As a part of the Calendar Year 2024 Medicare Physician Fee Schedule, the Centers for Medicare and Medicaid Services established Healthcare Common Procedure Coding System (HCPCS) Level I codes, also known as CPT® codes, to describe Principal Illness Navigation (PIN) services (Figure 2). PIN services include those that help patients diagnosed with high-risk conditions like cancer to identify and connect with appropriate clinical and support resources. These services are provided by certified or trained auxiliary personnel (e.g., patient navigator, certified peer specialist) and under the general supervision of a physician or other practitioner. These codes became effective January 1, 2024.
Figure 2: New CPT Codes for PIN Services

Establishing codes to identify and pay for navigation services supports the financial viability of and patient access to oncology navigation programs, while allowing utilization of patient navigation services to be tracked and assessed in the future.
Outlook for Oncology Navigation Services
The benefits of oncology navigation services are broadly accepted across stakeholder groups. Alternative payment models in oncology, such as CMMI’s Enhancing Oncology Model, often require oncology navigation services and provide an associated per-member per-month payment to enable practices to provide these services. As more providers and payers utilize PIN codes, policymakers and patient advocacy organizations will be able to assess outcomes among patients who received these services to establish best practices and standardize offerings.
Dive Deeper
Avalere has a dedicated coding team that can help stakeholders better understand the implications of the new CPT codes on reimbursement for oncology navigation services. Our team has extensive experience working in the oncology space and understands the unique needs of cancer patients. Connect with us to learn more about how Avalere can support your coding and reimbursement needs related to oncology navigation.
CPT ©2024 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
January 23, 11 AM ET
Learn More
