Strategic Imperatives for Skilled Nursing Facilities Preparing for New Payment System
Summary
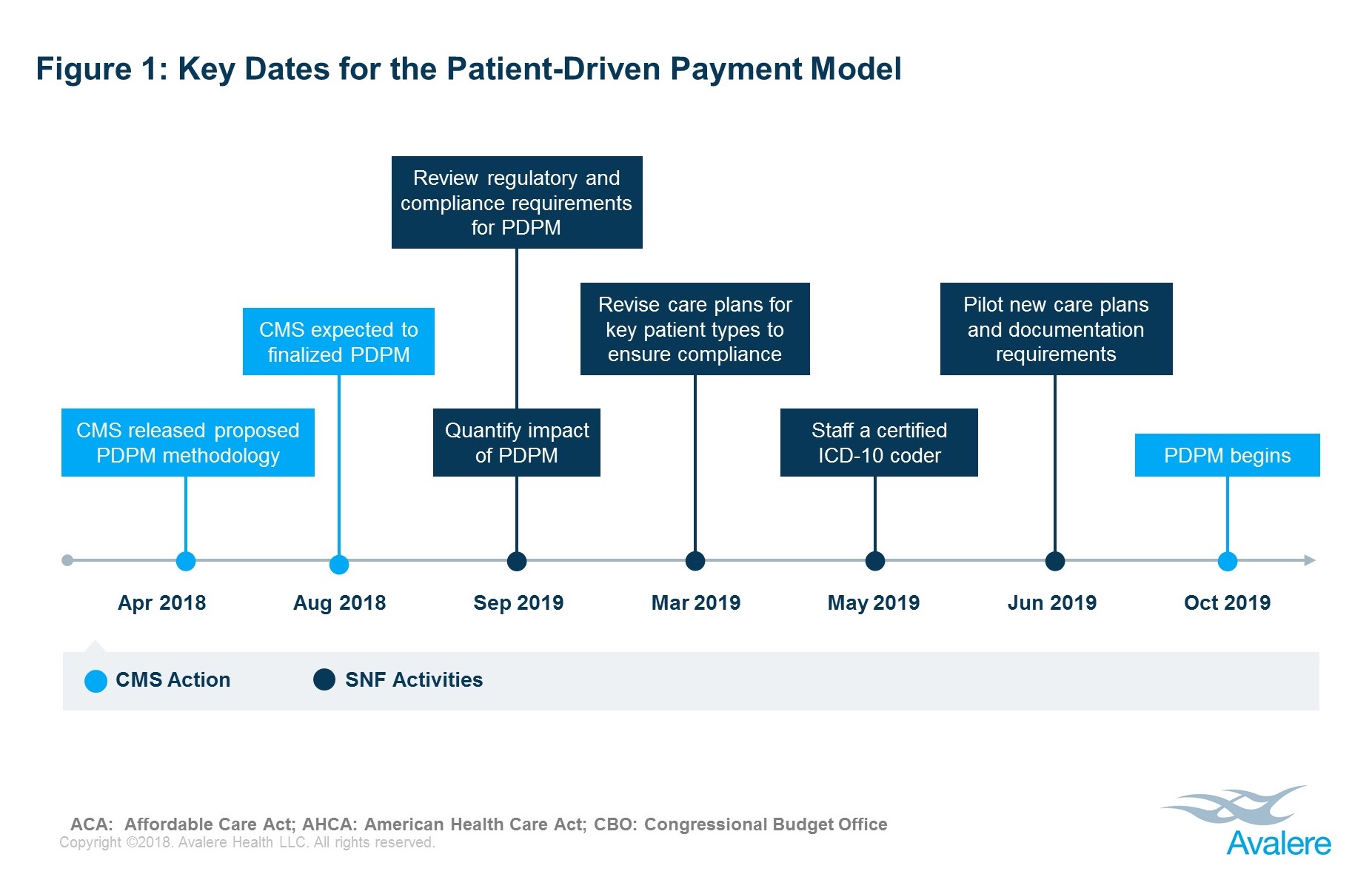
In August 2018, CMS is expected to finalize a proposed new payment methodology for skilled nursing facilities (SNFs) that would shift the focus from resource use to patients’ clinical needs.The new system, known as the Patient-Driven Payment Model (PDPM), would adjust payment based on patient care needs and characteristics. The new approach would replace the current Resources Utilization Group (RUG-IV) system beginning October 1, 2019. PDPM would maintain the current per diem payment rate, but it is designed to include more clinically relevant patient-driven factors. Most notably, PDPM would remove the provision of therapy minutes as a criterion for payment.
Although the implementation of PDPM would be budget neutral in aggregate, individual facilities may experience a change in total Medicare reimbursement under the new system. CMS compared current payments under RUG-IV to estimated payments under PDPM and found that Medicare reimbursement may decrease by roughly 40% for some SNFs but could increase by approximately 70% for other facilities.
Strategic Imperatives for Skilled Nursing Facilities
- Quantify Patient-Level Impact. PDPM has the potential to shift the average Medicare payment for individual patients. SNFs must evaluate how PDPM will impact the patient populations commonly treated in their facilities with a goal of understanding potential changes in reimbursement for these specific patient types, allowing facilities to align internal operations with the new reimbursement methodology.
- Develop New Documentation Expertise. Under PDPM, SNFs will need to document patient characteristics and needs in new ways. The primary reason for the SNF stay will be a key criterion of reimbursement. SNFs must have the expertise and skill set to not only identify the primary reason for the SNF stay, but also document it for reimbursement purposes.
- Focus on Medically Complex Nursing Care. PDPM removes the overarching focus on therapy present under the current reimbursement model. Highly specialized and skilled nursing services will be a greater focus under PDPM. SNFs must have the expertise and skill sets to provide these highly specialized services and accurately document patient characteristics and the care they have delivered.
- Align Care Delivery Strategy. PDPM trims reimbursement as a stay progresses, reflecting the fact that that level of care decreases throughout a SNF stay. SNFs must evaluate reimbursement rates and care guidelines under PDPM and adjust operations appropriately to ensure program compliance and effective cost management.
To learn more about how to prepare for PDPM, contact Erica Breese.
For more on Avalere’s services and capabilities, connect with us.
Learn More