A Deep Dive Into Hospice Utilization Trends
Summary
Avalere analysis reveals an opportunity to support more Medicare beneficiaries with hospice care, as evolving diagnoses and ALOS prompt reevaluation of program metricsThe Medicare Payment Advisory Commission (MedPAC) defines the Medicare hospice benefit as palliative and support services for beneficiaries who are terminally ill with a life expectancy of six months or less if the illness runs its normal course. The use of hospice services within the Medicare program has increased since 2013, driven by longer life expectancies and cultural shifts surrounding end-of-life care. Despite the growth in use, Avalere’s analysis suggests continued opportunity to support Medicare beneficiaries at the end of life.
Rise of Hospice-Eligible Beneficiaries in the United States
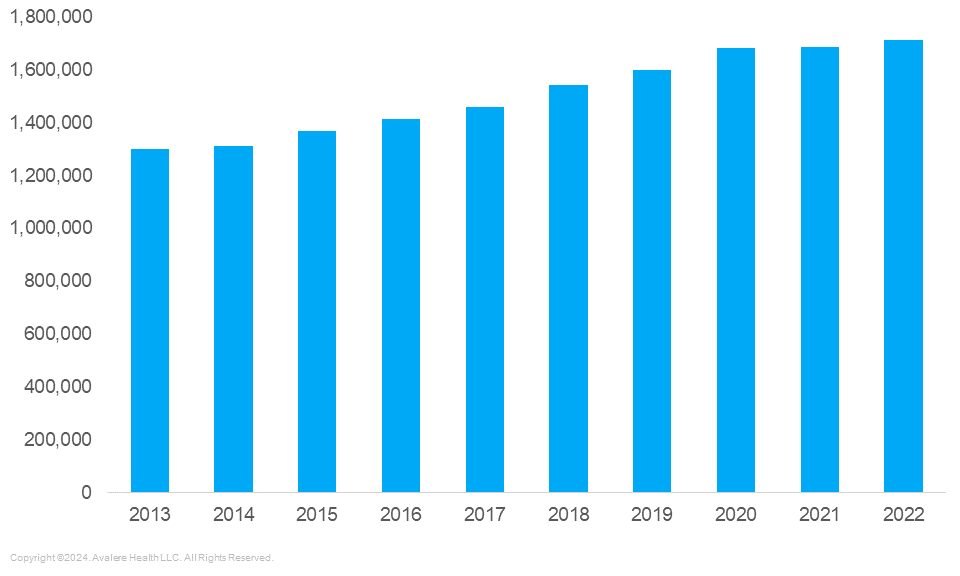
Between 2013 and 2022, as Baby Boomers aged, the total number of Medicare beneficiaries increased by nearly 25%, or 12.6 million enrollees. During that same period, hospice utilization outpaced Medicare growth, increasing by 32% (see Figure 1). This decade was characterized by a growing focus in the United States on improving conditions surrounding the final months of life, driving significant increases in hospice utilization.
Figure 1. Medicare Hospice Beneficiaries, 2013–2022
Rise of Hospice Utilization
Given the rise in hospice utilization in Medicare, the Centers for Medicare and Medicaid Services and MedPAC studied the appropriate use of hospice in order to prevent overuse and potentially wasteful healthcare spending. Both entities regularly report on quality, compliance, and spending findings to determine if additional action is needed.
One such finding is that between 2010 and 2022, average lengths of stay (ALOS) in hospice has increased as more individuals with different diagnoses enter the hospice program. MedPAC reported—and Avalere analysis confirmed— that beneficiaries with neurological disease diagnoses tend to have longer ALOS (155 days on average), while patients with diagnoses of cancer tend to have much shorter ALOS (55 days). We expect ALOS to continue to evolve as diagnoses associated with hospice use change. While preventing fraud, waste, and abuse in hospice is important to maintaining the integrity of the program, we expect ALOS to continue to fluctuate as the number of beneficiaries eligible for hospice increase or decrease in the future.
Addressing Unmet Need in Hospice
Despite rising utilization within the Medicare population, there remains a significant share of individuals who are eligible for hospice who are not enrolled in the program, reflecting an opportunity to provide support to individuals and families who may benefit.
Figure 2. Hospice Utilization in Medicare, 2013–2022

Figure 2 shows that 84% of eligible Medicare beneficiaries were enrolled in a hospice program in 2022, compared to 76% in 2013, signaling growth in the program. However, about 340,000 Medicare beneficiaries, or 16% of the addressable market, went without hospice care in 2022 despite being eligible for the program.
Conclusion
Avalere’s analysis shows that hospice penetration has reached nearly 85% of traditionally eligible diagnoses. Additionally, as the use of hospice matures, the mix of diagnoses and, in turn, the ALOS, evolves. While policymakers continue to explore the appropriate use of hospice, maturity of the program may necessitate rethinking what constitutes as an appropriate ALOS and how end-of-life benefits can be organized to offer more support to Medicare beneficiaries. While enforcement is important to prevent fraud, waste, and abuse, the industry might have to reconsider what the correct metrics are to evaluate utilization.
Methods
This analysis uses Medicare claims data to identify beneficiaries who may have been hospice eligible between 2013 and 2022. These beneficiaries were identified based on death without hospice use in the last six months of life as well as the presence of an inpatient, skilled nursing facility, or home health claim for one of the major hospice diagnosis categories in the 30 days before death. As utilization and diagnoses are only available for Medicare fee-for-service (FFS) beneficiaries, we applied the ratio of Medicare Advantage to FFS to estimate a total hospice eligible population.
Work With Us
Avalere is uniquely positioned to assist stakeholders in understanding the hospice industry and can leverage a bench of experts to investigate opportunities in this space. To speak with a hospice subject matter expert, connect with us.
Webinar | 2026 Part D Plan and Manufacturer Contracting Strategies
On Wednesday, October 30, at 1 PM ET, join our webinar to learn how Part D redesign and drug price negotiation will shape the Plan Year 2026 market, and what this means for manufacturers and plans.




