Assessing Changes in Prenatal Care During the COVID-19 Pandemic
Summary
COVID-related concerns influenced shifts in utilization and changes to the delivery of major pregnancy-related services. The expanded use of telemedicine in the maternal care continuum increasingly provided expectant patients with access to healthcare services while adhering to social-distancing guidelines.Since its emergence in late 2019 as a global pandemic, COVID-19 has impacted healthcare utilization and delivery. In March 2020, policymakers issued numerous social distancing restrictions and stay-at-home orders attempting to reduce the risk of virus exposure and transmission. These precautionary guidelines and federal policy changes led to major adjustments in the management of non-COVID-related care. Healthcare patterns reflect these changes, with noteworthy decreases in overall health care utilization and substantial increases of telehealth use. Though healthcare utilization and restrictions are beginning to revert to pre-COVID-19 levels, experts suggest that certain practices—such as telehealth and modified treatment modality schedules—may extend beyond the pandemic as the “new normal.”
Routine prenatal care (e.g., laboratory screenings, physical exams, ultrasound evaluations, counseling, risk assessments over the course of each trimester) has incorporated technology-based services to support risk reduction efforts. Traditional in-person appointments are an integral part of routine care for pregnancy. Typically, low-risk pregnant patients have a visit every 4 weeks until 28 weeks, every 2 weeks until 36 weeks, and weekly prior to delivery. Providers offering telemedicine are integrating a range of virtual services into pregnancy care, such as home monitoring to track key metrics over time (e.g., fetal heart rate, maternal weight, blood sugar) and virtual consultations for maternal-fetal issues, genetic counseling, and routine check-ups. These options help to reduce exposure to the virus and meet escalating patient demand for virtual care delivery.
Individuals with multiple chronic conditions and complex care needs are at increased risk of severe illness from the coronavirus if infected. Likewise, the stakes are much higher when coordinating care for high-risk pregnancies when defined by risk factors such as advanced maternal age, pregnancy complications, lifestyle choices, underlying health problems, multiple pregnancy, or history of pregnancy-related disorders. To assess changes in pregnancy care during the COVID-19 outbreak, Avalere performed analyses leveraging our data assets. This analysis can be expanded to include additional populations such as individuals enrolled in Medicare or reviewed more granularly to better understand disparities between certain racial/ethnic populations.
Methodology
Avalere analyzed telehealth utilization in Commercial (group, individual and exchanges) and Medicaid managed care markets using Inovalon MORE2 Registry®, a large scale, real-world multi-payer dataset consisting of medical, pharmacy, and lab claims as well as clinical data on more than 324 million de-identified patients. Avalere compared telehealth visits from 2019 (Mar–Dec) to 2020 (Mar–Dec) for enrollees with a live or cesarean birth to illustrate the potential impact of the COVID-19 pandemic. Avalere adjusted the analysis to account for any changes in claim sources within the data by employing a “same source” analysis that requires same providers and/or health plans to have submitted claims in both 2019 and 2020 to ensure that reported utilization changes are not driven by the addition or subtraction of claim sources over time.
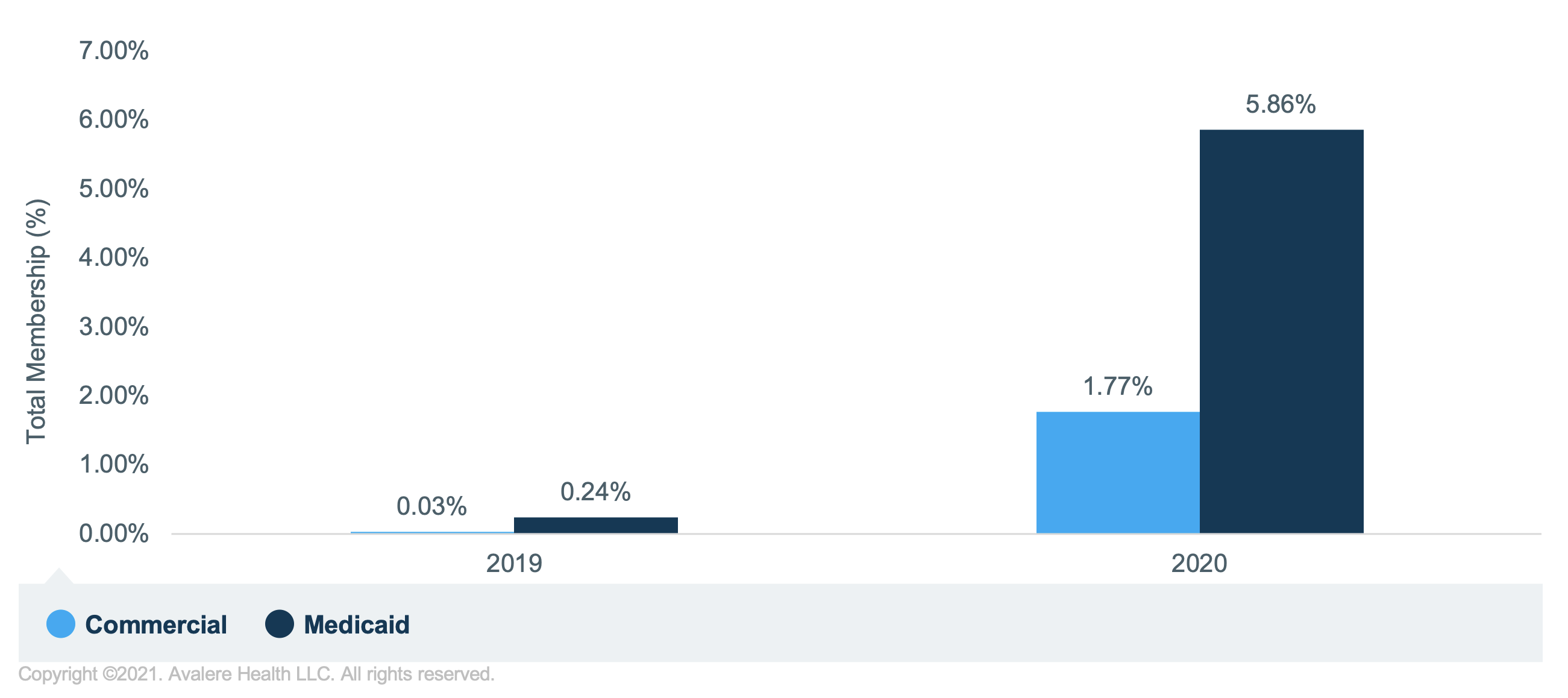
Increased Use of Telehealth and Telemedicine in Obstetrics
The effects of the pandemic have and will likely continue to influence various aspects of prenatal care, including telehealth. As providers continue integrating telehealth in obstetrics, patients can access care across various platforms. A review of telehealth utilization trends across Medicaid and Commercial populations highlights substantial increases in utilization for both groups between 2019 and 2020 (Figure 1). These patterns follow greater accessibility and reception as a valuable way to receive services, such as at-home monitoring, video visits, and remote check-ups with clinicians. In addition, the American College of Obstetricians and Gynecologists (ACOG) released a committee opinion for implementing telehealth in practice and advocating for expanding telehealth to ensure uninterrupted care for patients. The organization’s support of telehealth in obstetrics could facilitate expanded use and future innovation.
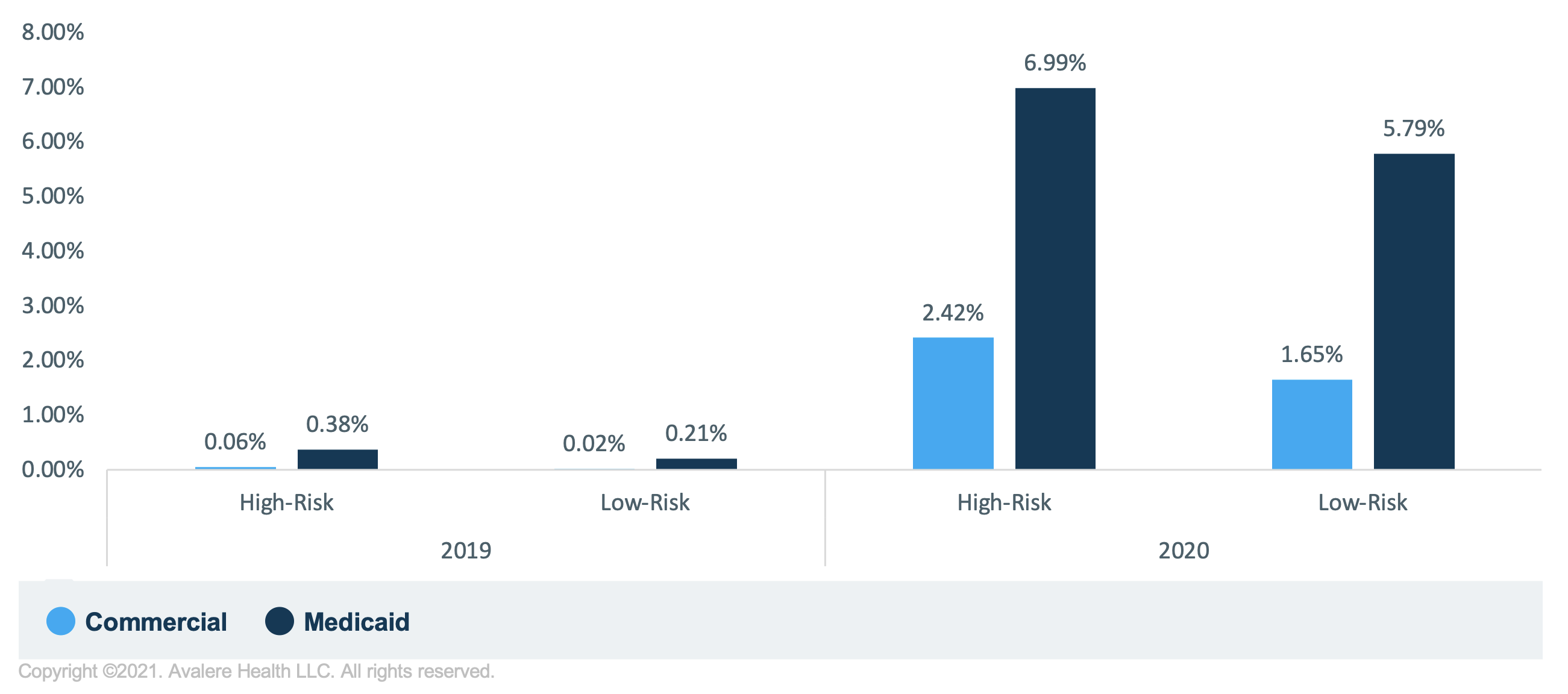
Moreover, high- and low-risk patients more often used telehealth in 2020 than 2019 in both Medicaid and commercial populations (Figure 2). Notably, among patients with telehealth visits, nearly a quarter were high-risk patients among the Medicaid population and over a fifth were among the commercial population. Within this analysis, the distribution of high-risk versus low-risk pregnancy were similar across racial groups with slightly higher percentages among Black (21%) and Hispanic (21%) patients in the Medicaid population when compared to White patients (17%). Among the commercial population, Black patients had a higher percentage of high-risk pregnancies when compared to White patients, 18% versus 12% respectively. This information warrants further research and is consistent with racial disparities observed in pregnancy risks and complications in the US.
On a broader scale, differences in the rates of pregnancy-related complications are also commonly observed across racial groups. On average, Black patients are 3–4 times more likely to die from pregnancy-related complications than any other racial group and are more likely to receive care from an underperforming hospital. For instance, Black patients are 3–4 times more likely to have pregnancy-related complications than any other racial group and are more likely to receive care from an underperforming hospital. Data from our analysis may point towards a much larger systemic problem likely exacerbated because of the pandemic.
| 2019 | 2020 | |||
|---|---|---|---|---|
| High Risk | Low Risk | High Risk | Low Risk | |
| Commercial | ||||
| Asian | 0.9% | N/A | 8.7% | 7.0% |
| Black | 0.5% | 0.5% | 7.4% | 5.7% |
| Hispanic | N/A | N/A | N/A | N/A |
| White | 0.1% | 0.1% | 9.4% | 6.2% |
| Medicaid | ||||
| Asian | 0.2% | 0.1% | 7.3% | 6.7% |
| Black | 0.2% | 0.1% | 7.1% | 5.9% |
| Hispanic | 0.5% | 0.2% | N/A | N/A |
| White | 0.5% | 0.3% | 7.0% | 5.4% |
For cells marked N/A, data were not available or no value was available for input.
Conclusion
Despite regulatory constraints requiring less social interaction and subsequently limiting in-person visits, the incorporation of telehealth-based services has allowed patients continued access to services during the pandemic. For maternity care providers, the prioritization of patient safety required the implementation of innovative strategies to reduce the spread of the novel coronavirus. Integrating telehealth-based approaches into prenatal care delivery is 1 way to increase healthcare access. Another method was highlighted in a March 2020 Frequently Asked Questions document released by ACOG, which focused on how providers were using modified obstetric visit schedules and alternative models (on a case-by-case basis), primarily for low-risk pregnancies during the pandemic.
The adjustments included reducing the number of in-person visits to 1 initial visit, anatomy ultrasound visit, and a 26th, 28th, and 39th week check-in, and tailoring frequency of services to patient needs. Currently, revised prenatal care schedules are increasingly being considered to provide patients with a flexible option for care delivery and reduce associated healthcare costs. Adjusting prenatal care schedules as well as utilizing telehealth in pregnancy care delivery allow patients to receive consistent and tailored care across a range of healthcare platforms. While the current regulatory landscape supports greater usage, recent research conducted by George Washington University’s Department of Obstetrics and Gynecology also notes the effectiveness of telehealth on health outcomes outside of the pandemic environment.
Providers, health insurance payers, and maternal health advocacy groups should consider how pandemic-related shifts in care may influence patient outcomes, informed care decisions, prenatal and postpartum coverage, and quality of care measures. Avalere can assist stakeholders with further analysis in 1 or all of the following ways:
- Developing innovative pilot programs focused on achieving healthier outcomes in prenatal and postpartum care (e.g., telehealth/alternative care programs, outreach/educational programs, shared decision-making and social determinants of health focused initiatives)
- Assessing telehealth’s role in increasing access to care and its role in the continuum of care for maternal and child health
- Advising on key maternal health policy and regulatory landscape updates
- Analyzing prenatal and postpartum care utilization specific to a plan’s enrollment or comparative analysis between specific lines of business (i.e., Medicaid, Medicare, and commercial)
- Exploring how existing disparities widened during the pandemic using data-driven analyses to identify barriers to accessing high-quality care and support quality improvement and disparities reduction initiatives
Avalere will continue to monitor the impact of the COVID-19 pandemic on maternal and child healthcare utilization and care delivery modalities.
To receive Avalere updates, connect with us.
Avalere Health is an Inovalon company, a leading provider of cloud-based platforms empowering data-driven healthcare. We believe in the power of data, informing actionable insights, delivering meaningful impact, and driving stronger patient outcomes and business economics.




