Healthcare Organizations See Reduction in ED Visits and Inpatient Admissions when Focusing on Value
Summary
Avalere worked with a healthcare organization to assess the impact of their quality improvement program over a 4-year period. The organization prepared primary and specialty care providers/practices to transition from fee-for-service (FFS) to value-based payment arrangements. Avalere’s analysis found participation in the program led to a reduction in both emergency department (ED) visits as well as inpatient (IP) admissions over the period reviewed.Avalere was engaged by a healthcare organization that treats approximately 100,000 beneficiaries in the southeastern US to assess the impact of participation in a quality improvement program on certain measures. The organization supplied practices with the quality improvement expertise and resources to improve care and reduce unnecessary costs.
Avalere examined the impact of participating in the program and the respective impact on IP admissions and ED visits over the duration of each participation year. Avalere conducted the analysis using Medicare FFS claims data available under a research-focused data use agreement.
- Number of Inpatient Admissions: This measure identifies acute inpatient hospital claims to analyze the number of hospitalizations per 100 beneficiaries per year. Constructing the measure for the participation group, Avalere was able to determine that IP admissions had been reduced by 5.2% in year 1, by 5.8% in year 2, and by 4.7% in year 3.
- Number of ED Visits: This measure used ED revenue and current procedural terminology codes to identify ED visits. This measure is then reported as number of ED visits per 100 beneficiaries per year. Constructing the measure for the participation group Avalere was able to determine that ED visits had been reduced by 3.1% in year 1, followed by a reduction of 2.7% in year 2, and finally a reduction of 5.8% in year 3.
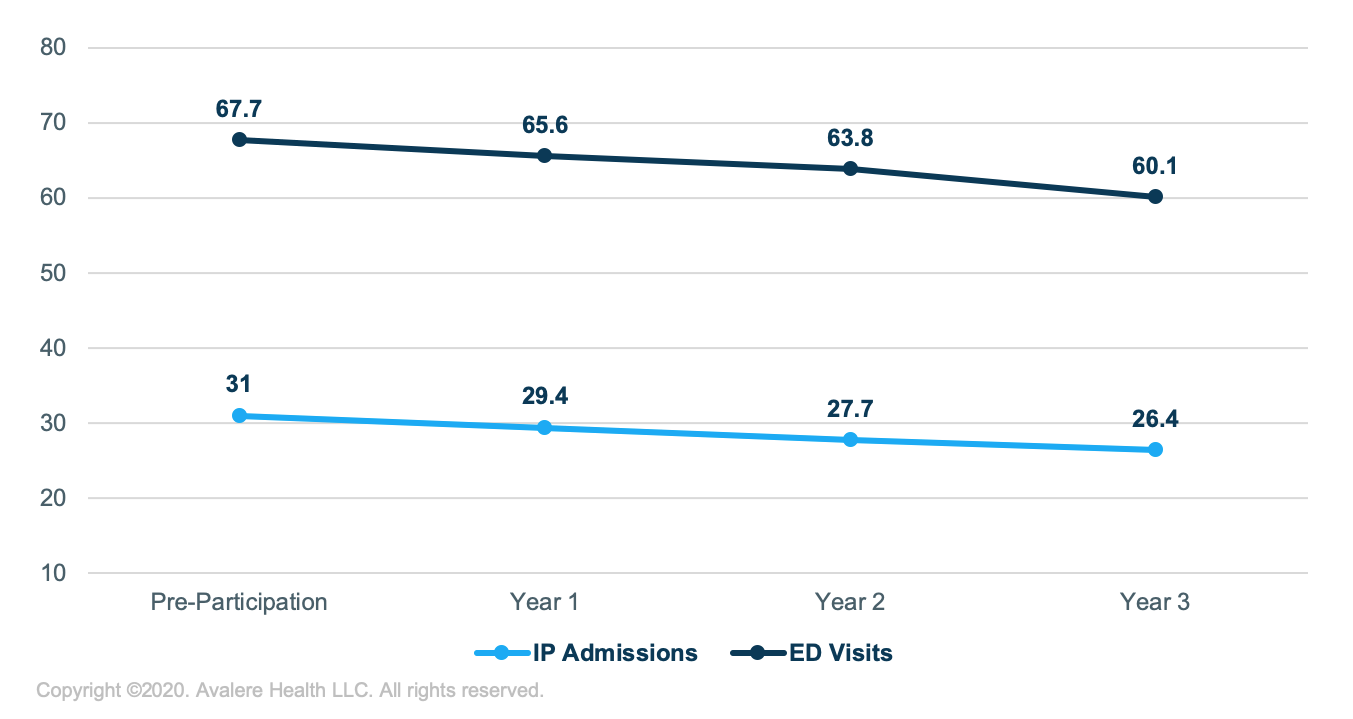
Overall, Avalere’s analysis suggests that a result of participating in the quality improvement program was notable reduction in ED visits and IP admissions, which would suggest a translation to reduced costs for these providers.
To learn more about our modeling work, connect with us.
Find out the top 2020 healthcare trends to watch.







