Mental Health Treatment Integration Can Offer Cost Savings
Summary
Adequately treating mental health disorders can cut overall costs, including those from comorbidities, despite access barriers and high comorbidity expenses.Mental health continues to represent one of the largest and most pressing challenges to the American healthcare system. In 2021, over one in five US adults experienced a mental illness, and 5.5% experienced a serious mental illness. Americans face significant barriers in accessing mental healthcare, with downstream implications for overall health outcomes, comorbidities, and system expenditures.
Avalere conducted two analyses investigating the relationship between mental health conditions, comorbidities, and overall spending. Avalere also conducted a third analysis highlighting geographic variations in reimbursement in mental health treatments.
Analysis 1: Comorbidities of Major Depressive Disorder (MDD) with Anhedonia
Avalere investigated the types of comorbidities linked with anhedonia in patients with MDD. Anhedonia is the inability to experience joy or pleasure, which is a common but underdiagnosed symptom of mental health conditions like depression. Anhedonia is a predictor of negative long-term outcomes such as suicide and poor response to treatments. There continues to be unmet needs in treatment options for patients with anhedonia, which is a high-risk and core symptom of MDD.
Avalere identified the top eight primary and secondary diagnoses among patients with MDD with anhedonia among Medicare fee-for-service (FFS) beneficiaries in calendar year (CY) 2022. These comorbidities are:
| Primary | Secondary |
|---|---|
| Hypertension | Hypertension |
| Disorders of Lipoid Metabolism | Disorders of Lipoid Metabolism |
| Anxiety and Other Psychiatric Disorders | Anxiety and Other Psychiatric Disorders |
| Bipolar Disorder | Thyroid Disorders |
| Diabetes with Complications | Diabetes with Complications |
| Thyroid Disorders | Chronic Obstructive Pulmonary Disease, Bronchiectasis, and Other Asthma |
| Dementia, Except Alzheimer’s Disease | Coronary Artery Disease |
| Schizophrenia and Other Psychosis | Dementia, Except Alzheimer’s Disease |
In Medicare FFS, common comorbidities such as hypertension and diabetes were chronic conditions expected with the age of the population. However, mental health disorders such as anxiety, bipolar disorder, or schizophrenia were also prevalent. This indicates a linkage between MDD with anhedonia and these mental health diseases, highlighting the need for an integrated treatment approach. This analysis demonstrates that creating access to integrated mental healthcare may increase the availability of health services and enhance patient outcomes.
Analysis 2: Expenditures Associated with Major Depressive Disorder
Another Avalere analysis focused on MDD, a serious mental health condition characterized by a persistent and intense feeling of sadness or a lack of interest in external stimuli that impacts daily functioning and quality of life. Avalere’s analysis demonstrated significant increases in medical expenditures for patients with comorbidities when those patients did not receive adequate mental healthcare for MDD.
In all comorbidity subgroups analyzed (diabetes, schizophrenia and bipolar disorder, and congestive heart failure), total expenditures in the adequately treated group were better controlled in the 12 months following diagnosis compared to the inadequately treated group. Specifically, total expenditures related to the comorbid condition were 6.6%–8.5% lower in the adequately treated group within the same 12-month period.
This analysis demonstrates that mental health conditions currently place a significant economic burden on the US healthcare system. Addressing the cost of mental health conditions and comorbidities requires an integrated care approach with mental health screening, early intervention, and collaborative care.
Figure 1: Baseline Comparison for All-Cause Medical Expenditures by Comorbidity
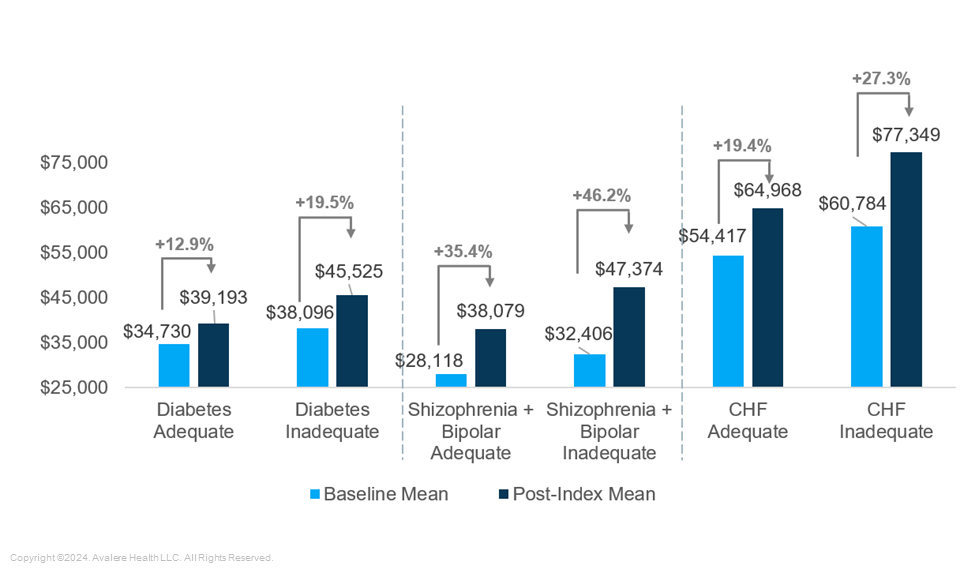
Adequate: Patient had four psychotherapy visits in the first 12 weeks after diagnosis and filled antidepressant prescription for at least 84 of the first 144 days; Inadequate: Patient did not meet psychotherapy or prescription criteria; Baseline Mean: 12 months preceding the initial diagnosis of MDD; Index Date: The date on which the first MDD diagnosis was made; Post-index Mean: 12 months following the initial diagnosis
Analysis 3: Geographic Variations in Reimbursement
Reimbursement affects access to innovative mental treatments and services. Avalere’s analysis compared utilization trends among Medicare FFS Part B beneficiaries in 2021 and 2022 to understand differences in administration of a newer, branded MDD drug. Findings demonstrated that there were geographic differences in reimbursement: Medicare payment was highest in Pacific and East Coast states (Texas and Arkansas were notable exceptions, with higher payment). These findings indicate that patients residing in these areas may have greater access to specific treatments, based on provider willingness and capacity to prescribe.
Next Steps
Mental health has often been viewed independently of other health conditions, but these findings reveal its association with other high-cost conditions. Avalere’s research also exposes the significant barriers that many Americans face in treating their mental health, and the overall system expenditures that the associations between this lack of access and mental and physical comorbidities create. This analysis highlights that fostering broader access to mental healthcare that is consistent, thoughtful, and integrated with broader physical care delivery will create a path for overall improvement of patient outcomes and reduction in system burden and expenditure.
Avalere experts can help you understand the dynamics in the mental health space, the potential impacts on your business, and opportunities for involvement. To learn more about how Avalere can help, connect with us.
Methodology
Avalere performed this analysis using 100% Medicare FFS claims, accessed by Avalere via a research collaboration with Inovalon, Inc., and governed by a research-focused CMS data use agreement. This includes the 100% sample of Medicare Part A and Part B Medicare FFS claims data.







