Overview: Balance Billing or Surprise Medical Bill Reform
Summary
Surprise and balance billing reform efforts have been a subject of ongoing debate at the federal level.Introduction
The terms “surprise bill” and “balance billing” are generally used to describe when a patient unknowingly receives care from an out-of-network provider—usually during an emergency or as part of a planned medical procedure at an in-network facility—and is billed for the difference between the sum of what he and the insurance company paid and what the provider bills. State legislation addressing balance billing has been adopted to varying degrees across 30 states. Federal legislation, however, has failed to reach the floor of the Senate or House for a vote.
Applicability of Surprise Billing
Legislative approaches to surprise billing are generally not written to encompass or inhibit all out-of-network billing but are targeted toward specific situations and settings of care that policymakers believe have the greatest negative impact on patients. These approaches typically target two forms of billing:
- Emergency medical bills: In emergency care situations, a person may receive care at a facility or from providers that are outside their insurance network or at an in-network facility where services are provided by an out-of-network provider. In these situations, a person receives a bill for not only cost sharing (copay, coinsurance, and deductible), but also for the additional amount the provider charges above the amount paid to the provider by their insurer for out-of-network care.
- Surprise medical bills: In a circumstance involving a scheduled procedure, sometimes a facility is in the insured patient’s network, but one or more of the providers delivering care, such as an anesthesiologist or pathologist, are not included in that patient’s network. Medical surprise billing proposals are typically targeted toward anesthesiology, radiology, and pathology services.
As a majority of legislation targets both emergency and surprise medical bills, for the purposes of clarity Avalere will refer to all legislation as simply “surprise billing.”
Approach to Surprise Billing Rate Negotiations
Congressional proposals to date generally rely on one of two mechanisms to set the rates paid to providers for out-of-network surprise bills: independent dispute resolution (IDR) and payment benchmarks.
Should legislation pass, a potential compromise policy could be a hybrid approach, through which surprise medical bills use a dollar threshold above which the plan and provider enter into an IDR process and below which the payment defaults to a payment benchmark. These approaches are illustrated below:

Federal Reform Proposals and Implementation
To date, legislative packages passed to address the ongoing public health emergency related to COVID-19 have not included provisions specific to surprise billing. Unless Congress chooses to reopen a broader healthcare debate in general or as part of a discussion over financing COVID-related reforms, near-term action on surprise billing is unlikely at the federal level.
As legislation is expected to have an implementation timeline of at least 2 years after the bill’s enactment, a compromise reached in 2021 would likely be implemented no earlier than 2023, with legislation passed later in 2021 potentially seeing implementation in 2024.
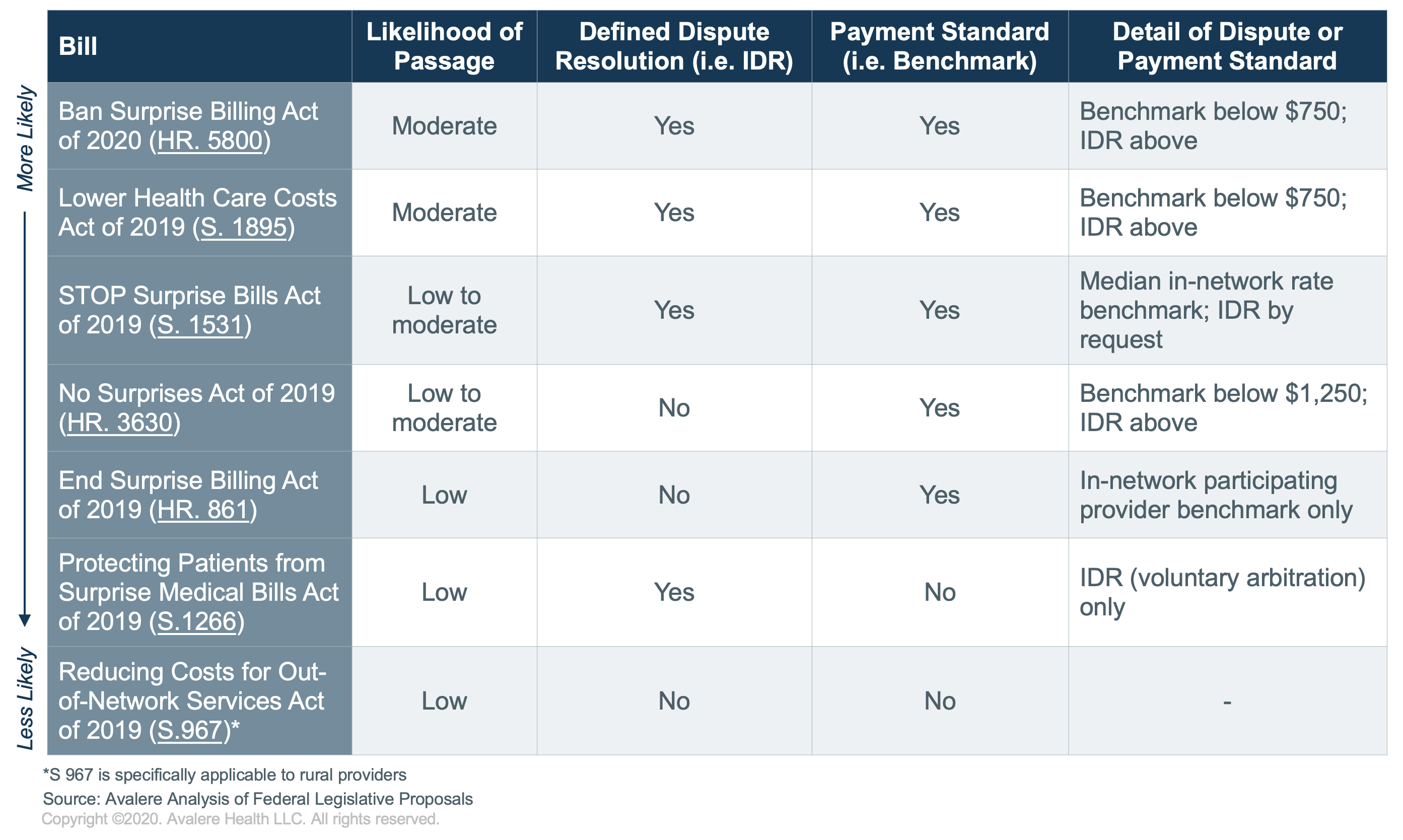
The table below highlights the various approaches to surprise and balance bill reform proposed by various congressional stakeholders to date:
In total, the environment for surprise billing reform remains complicated across the legislative and stakeholder landscape. While the long-term outlook will continue to favor some type of legislative action regarding surprise billing, stakeholder division and competing priorities are likely to delay immediate action.
Funding for this research was provided by Churchill Capital. Avalere maintained full editorial control.
To receive Avalere updates, connect with us.







