Stakeholders Address Disparities in Breast Cancer Screening
Summary
Avalere found disparate breast cancer screening rates by race/ethnicity and insurance type. Stakeholders are seeking to address barriers to patient access.Guidelines and Patient Access
Since 2016, the US Preventive Services Task Force (USPSTF) has recommended biennial breast cancer screening using mammography for women ages 50–74 who are at average risk for breast cancer with a “B” grade. In April, USPSTF released an updated draft recommendation that would reduce the age to start screening mammography to 40 years.
Under the Affordable Care Act (ACA) preventive services coverage mandate, most commercial health plans are required to cover—with no cost-sharing—services recommended by the USPSTF with an “A” or “B” grade. The requirement also applies to Medicaid expansion populations.
With the recent Braidwood v. Becerra ruling that removes the enforcement of coverage of cancer screening guidance from USPSTF, and poses potential impact on future access to preventive care and cancer screening services, Avalere examined breast cancer screening utilization in the US before this ruling.
Real-World Evidence of Screening
Avalere performed a retrospective claims analysis to identify utilization of breast cancer screening services since the preventive services coverage mandate went into effect. Using 2018-2019 claims data, we identified the number of women ages 50-74 who received at least one breast cancer screening vs. those who did not receive screening. We included a 2-year scan of claims prior to the COVID-19 pandemic to not introduce additional barriers to access existing during that time.
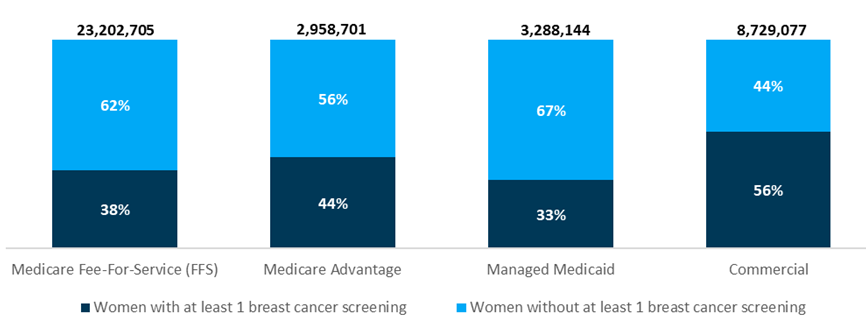
Fewer than half of women 50-74 years of age with Medicare fee-for-service (FFS) (38%), Medicare Advantage (44%), or Medicaid managed care (33%) received breast cancer screening (see Figure 1). Commercial plans had the highest percentage of women who received screening (56%), which may be due to the ACA’s preventive services coverage mandate. Even with USPSTF guidance and ACA support for access in place, what were potential barriers to access that are possibly still in existence today?
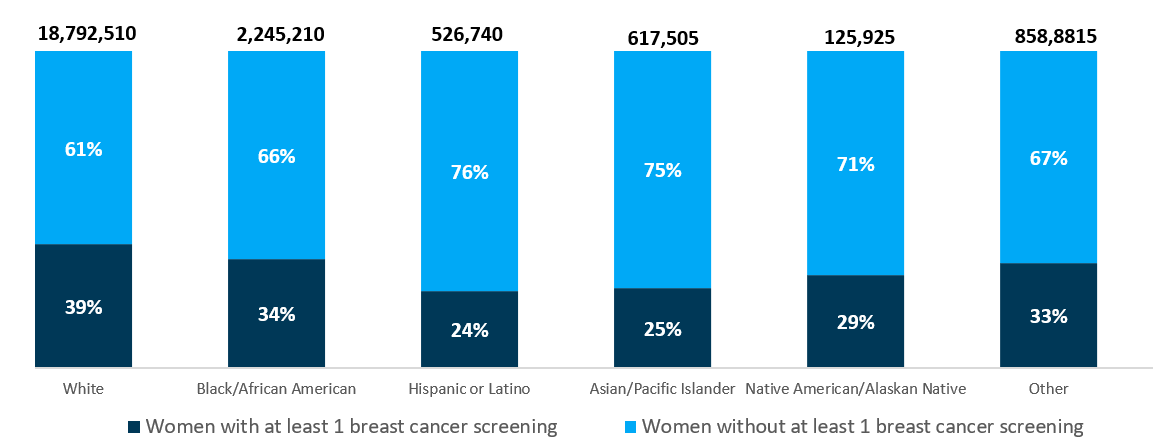
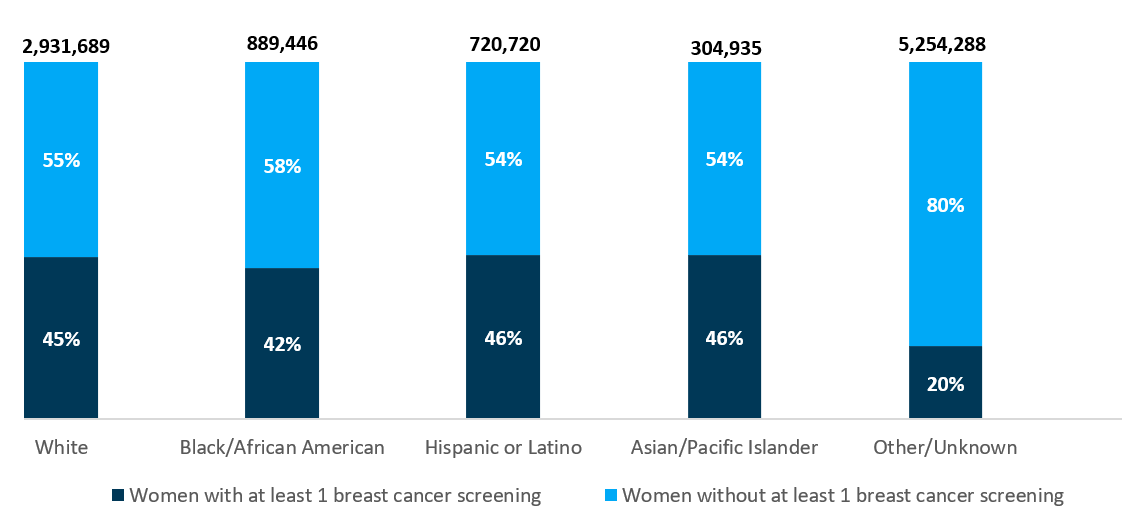
Avalere also analyzed rates of breast cancer screening in the Medicare FFS population and other payer types by race/ethnicity. Among women with Medicare FFS, Hispanic/Latino women had the lowest screening prevalence (24%), closely followed by Asian/Pacific Islander women (25%) (see Figure 2). Among women insured through other payer types, those in the Other/Unknown group had the lowest screening prevalence (20%), less than half that of women in other groups (see Figure 3).
Current Barriers
Although we do not expect to see 100% screening in women in this analysis, because some may not qualify for screening based on risk or due to personal choice, the majority did not receive screening in 2018-2019.
Avalere conducted separate primary research with patients with breast cancer and supplemented findings with literature to understand barriers to accessing screening. Barriers to screening include unreliable transportation, geographic isolation, cultural and language barriers, low health literacy, mistrust in the medical system, cost, and lack of insurance, all of which are exacerbated by systemic racism.
As the data shows there may be multiple barriers to solve, there are stakeholders in healthcare already taking actions to address these barriers.
Stakeholder Actions
The draft recommendation proposed by USPSTF in April align with breast cancer screening guidelines from the National Comprehensive Cancer Network (NCCN), a not-for-profit alliance of 33 leading cancer centers.
The NCCN 2023 Annual Conference, which took place shortly before USPSTF released its draft recommendation, featured presentations on barriers to breast cancer screenings and measures that may be used to address these barriers.
A molecular diagnostic company discussed how multi-cancer early detection testing can detect multiple cancer types using a blood draw and could help expand access to screening for underserved populations. Another presenter, a large academic medical center, demonstrated how mobile screening programs (including mammography) improved patient access to oncology care in their area, highlighting the importance of community outreach and engagement. Attendees also highlighted the Dana-Farber Cancer Institute’s Cancer Care Equity Program (CCEP), which aims to reduce disparities in cancer outcomes and improve access to preventive services through community outreach and educational programs.
Key healthcare stakeholder such as screening companies, advocacy groups, and health care systems are collaborating on community-based strategies such as establishing mobile clinics, creating educational materials, ensuring coverage of screening tests for those uninsured, and addressing system biases to address barriers in cancer screening.
Conclusion
Through the concerted efforts of these stakeholders in their communities, access to guideline-recommended screening is improving. Efforts like these may improve patient outcomes, long-term medical cost, and reduce mortality rates. This is true especially for the underserved patient population.
Our analysis of claims data and literature review found that barriers to breast cancer screening may go beyond payer coverage and affordability. Stakeholders in this space should monitor efforts to address these barriers and their impacts on patients.
Methodology
Avalere performed this analysis using 100% Medicare FFS, Medicare Advantage, Medicaid managed care, and commercial claims, accessed by Avalere via a research collaboration with Inovalon, Inc., and governed by a research-focused Center for Medicare & Medicaid Services data use agreement. This includes the 100% sample of Medicare Part A and Part B Medicare FFS claims data. The commercial claims database is populated by providers which are contracted and are not sampled to be nationally representative but rather rely on a large national convenience sample.
January 23, 11 AM ET
Learn More


