What is the CMS Innovation Center?
Summary
The CMS Innovation Center offers policymakers a nimble, non-legislative pathway to experiment with new methods of care delivery, payment, and reimbursement in Medicare and Medicaid.What Is the CMMI’s Mission?
The Affordable Care Act (ACA) gives the Centers for Medicare & Medicaid Innovation Center (CMMI) broad authority to test innovative payment and service delivery models through demonstrations that aim to reduce program spending while maintaining or improving quality of care. The Secretary of the Department of Health & Human Services (HHS) may expand a model nationwide if it does not limit the coverage or provision of any benefits. The model must either reduce spending without reducing the quality of care or improve the quality of care without increasing spending.
How Do Model Demonstrations Work?
All CMMI models move through two phases:
- Phase I, Model Testing and Evaluation: In consultation with the chief actuary of the Centers for Medicare & Medicaid Services (CMS), the CMMI evaluates model performance based on its impact on quality of care and spending. This phase typically lasts 5 years.
- Phase II, Model Expansion Determination: Based on the results of Phase I, the Secretary of HHS decides whether to expand the scope and duration of the payment or delivery model. A successful model can also be extended to all of Medicare, Medicaid, or the Children’s Health Insurance Program (CHIP) through rulemaking.
On What Topics Do the Models Focus?
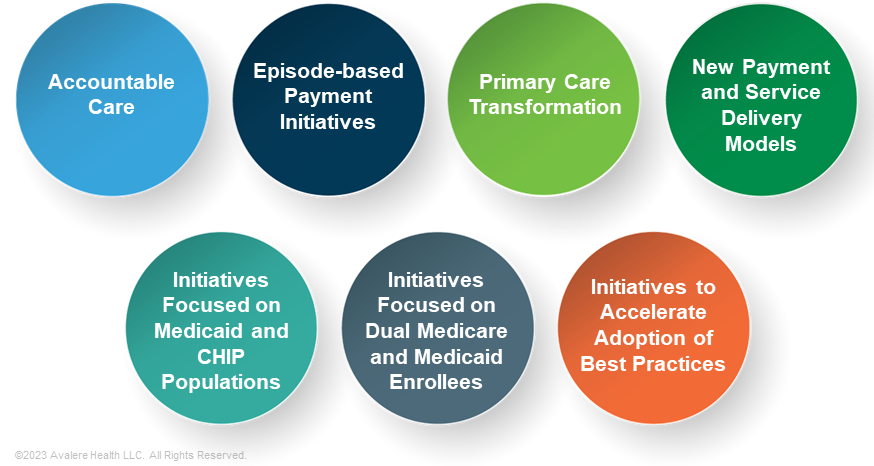
The CMMI classifies its care delivery models into seven categories:
How Much Flexibility Does the CMMI Have to Test Models?
Through demonstrations, CMMI has authority to waive key Medicare program requirements, including:
- Anti-Kickback Statute
- Civil Monetary Penalties Law
- Stark Self-Referral Law
- Beneficiary freedom of choice
- Part B drug reimbursement methodology
- Scope of covered benefits
How Does the CMMI Select Models to Test?
Models must serve populations for which “deficits in care” lead to poor clinical outcomes or potentially avoidable expenditures. The ACA also requires the CMMI to prioritize models that have the potential to improve the coordination, quality, and efficiency of healthcare services.
What Are the Biden Administration’s Priorities for the CMMI?
In 2021, the CMMI launched a strategy refresh to achieve equitable health outcomes. It is organized into five objectives:
- Increasing the number of people in care relationships that are accountable for quality and total cost
- Embedding health equity into every aspect of CMMI models
- Supporting innovation that enables integrated, person-centered care
- Addressing healthcare prices and reducing unnecessary care
- Aligning CMS priorities and policies and engaging external stakeholders to achieve the other four objectives
Have CMMI Models Reduced Costs?
Over the past decade, the CMMI has implemented more than 50 models, most of which have not reduced government costs. Between 2017 and 2026, Avalere estimates that the CMMI will produce $9.4 billion in net losses to the federal government. Aside from costs associated with CMMI operations, the estimated losses are largely from models that did not generate expected savings and models that did generate savings but shared those savings with participants or made bonus payments that ultimately cost CMS more than they earned. Experts have also expressed concerns that the savings evaluation method might not have captured true savings adequately.
To learn more about how the CMMI affects aspects of healthcare, connect with us.






