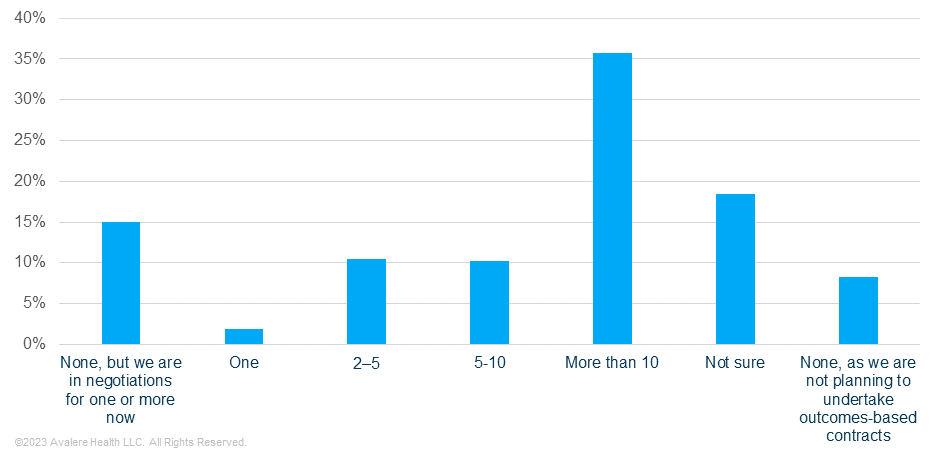
Survey Finds 58% of Payers Use Outcomes-Based Contracts
Summary
In 2022, over half of payers had at least one outcomes-based contract (OBC) and used claims-based outcomes, despite acknowledging the limitations of using claims to measure clinical benefit.In January 2023, Avalere conducted an online survey of 46 US-based health plans to assess their current awareness, use, experience, and attitudes toward OBCs during the 2022 plan year. Avalere has conducted this survey for five consecutive years, with some modifications to questions and inclusion criteria over time.
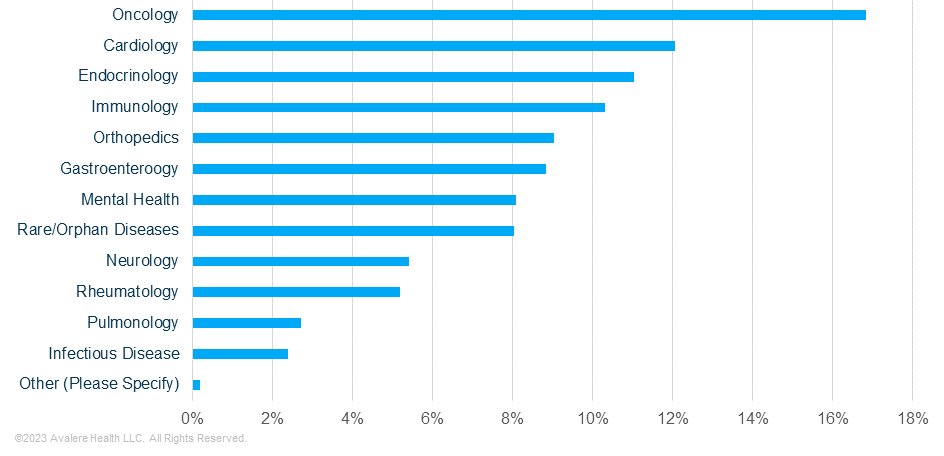
The survey indicates that 58% of surveyed payers had at least one OBC in place during the 2022 plan year (Figure 1). Respondents who are utilizing at least one OBC indicated oncology, cardiology, and endocrinology as the top therapeutic areas in which they utilized OBCs in 2022 (Figure 2). In addition, the majority of respondents said they are using OBCs for “mostly new products, but some existing products,” reflecting growing interest among stakeholders to align payment with clinical benefit, particularly for new products that have limited real-world clinical benefit.
Over seventy percent (74%) of payers with at least one OBC indicated they prefer contracts with both claims-based and clinical outcomes. However, over half of the respondents (53%) noted that they do not feel claims-based outcomes are a good proxy for clinical benefit. Claims-based measures are typically easier to track because they leverage information that plans and PBMs are already gathering, rather than clinical outcomes that may need to be tracked specifically for an OBC. Clinical measures can be more difficult to track if they require new data infrastructure and pose an additional administrative burden on providers and other stakeholders. Therefore, while clinical outcomes may better reflect clinical benefit, claims-based outcomes are more practical. As noted in Avalere’s webinar, The Evolving Cell & Gene Therapy Market, alignment among stakeholders on appropriate metrics of value that are also meaningful measures of clinical benefit is among the barriers to value-based care.
Methodology
Avalere conducted an online survey of US health plans between February 14 and February 20, 2023. Respondents were recruited from a comprehensive panel of health plan representatives and then screened to determine eligibility to participate, requiring that individuals be a decision-maker or influencer in their organization, identifying 46 qualified respondents. The panel’s overall size and distribution by plan membership, type, and geography reflect the health plan landscape at large, representing national and regional plans, and integrated health systems. Avalere weighted responses based on self-reported covered lives.
What Comes Next?
Avalere will release a comprehensive report detailing findings from the full survey in the coming weeks. The report will be available to subscribers of Avalere’s Federal Policy 360TM.
Avalere’s experts in innovative payment models can help you understand the evolving OBC landscape. To learn more about the potential impact of OBCs on your business, opportunities for involvement, and how Avalere can help, connect with us.





