Most Women with Cervical Cancer Were Not Screened Before Diagnosis
Summary
An Avalere analysis shows that those who had received cervical cancer screening within five years prior to diagnosis were diagnosed at relatively younger ages.Background
The American Cancer Society (ACS) and the US Preventive Services Task Force (USPSTF) have both issued recommendations for cervical cancer screening frequency across age groups. Typical screenings for cervical cancer include a Papanicolaou (Pap) test and/or Human Papillomavirus (HPV) test. Recommendations from both organizations are similar, although USPSTF recommends screenings to begin at age 21 and the ACS at 25.
Figure 1. ACS and USPSTF Screening Recommendations Across Age Groups
| mmAgemm | 2020 ACS | 2018 USPSTF |
|---|---|---|
| 21–24 | No screening | Pap test every three years |
| 25–29 | Pap test every three years, HPV test every five years, or HPV/Pap cotest every five years | Pap test every three years |
| 30–65 | Pap test every three years, HPV test every five years, or HPV/Pap cotest every five years | Pap test every three years, HPV test every five years, or HPV/Pap cotest every five years |
| >65 | No screening if a series of prior tests were normal | No screening if a series of prior tests were normal and not at high risk for cervical cancer |
Source: National Cancer Institute. ACS’s Updated Cervical Cancer Screening Guidelines Explained. 2020.
Despite the Affordable Care Act (ACA) requirement that most commercial health insurers provide coverage of women’s preventive healthcare (including cervical cancer screenings) with no cost sharing, most women are not receiving cervical cancer screenings in compliance with recommendations. There are notable disparities by insurance type (e.g., commercial vs. Medicaid) and age.
Cervical cancer is the fourth most common cancer in U.S. women aged 15-44. The mortality rate for Black and Native American women is approximately 65% higher than for White women. Disparities in survival rates also exist. Surveillance, Epidemiology, and End Results (SEER) data from 2014 to 2020 shows that Non-Hispanic Black women had the lowest five-year survival rate (58.1%). Additionally, younger women (15-39) have the highest survival rates, while women 75+ have the lowest.
Avalere’s Analysis
Methodology
Avalere researched the utilization of recommended cervical cancer screening in women, prior to a cervical cancer diagnosis. Avalere performed a retrospective analysis of women 26+ years of age who were newly diagnosed with cervical cancer in 2021-2022, and whether they were screened for cervical cancer in the five years prior to their diagnosis (age 21+ years), to capture the age range for screening in guideline recommendations. Avalere conducted this analysis using a convenience sample of Managed Medicaid, commercial insurance, and Medicare Advantage adjudicated claims. The analysis also looked specifically at women continuously enrolled in the insurance type for the analysis timeframe to ensure capture of all testing. Since the screening recommendations do not recommend regular screening past 65, the Medicare FFS population was not included.
Findings
The analysis revealed that around 29% of the approximately 1,500 women aged 21+ years in the sample received at least one screening Pap test in the five years preceding their diagnosis. In this group, 82% (N=1,202) of women were in the age group 21-65 years recommended for screening. The remaining women 18% (N=262) were older than age (aged 65+) for general population recommendations for screening, but did receive screening. Despite current recommendations for Pap tests every three years, the majority of the women (approximately 70%) in this sample did not undergo any screening Pap test within the five-year period preceding diagnosis.
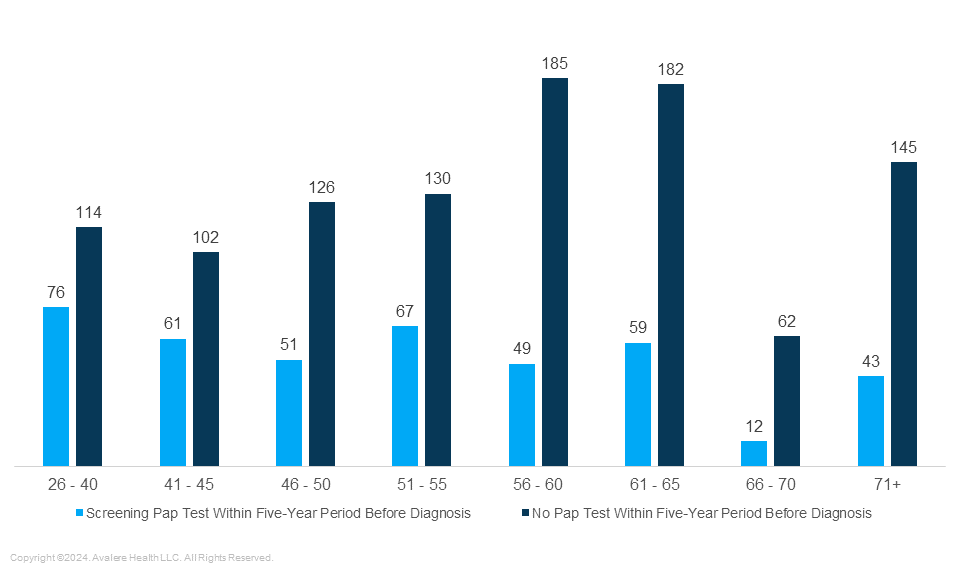
This analysis further showed that those receiving regular Pap tests were diagnosed at younger ages, with the highest number of diagnoses occurring in the 26–40 age range. Conversely, in the group that did not receive a screening Pap test in the five years prior to diagnosis, the number with a diagnosis increased with age, peaking in the 56-60 age group. The analysis also found 23% of women aged 71+ that were diagnosed with cervical cancer also underwent screening, which may have been indicated based on meeting personal criteria. Since age and severity at the time of diagnosis are directly correlated with survival in cervical cancer, diagnoses at older ages may be concerning with regards to outcomes. Additionally, as the likelihood of comorbidities increases with age, overall treatment costs may rise for women diagnosed in older age cohorts.
Figure 1. Number of Women Diagnosed with Cervical Cancer in 2021–2022 That Received Screening Within the Five-Year Period Prior to Diagnosis, Continuously Enrolled, Across Age Groups (N=1,464)
The analysis did not find any meaningful difference in the presence of metastatic cancer (early vs. advanced). However, metastatic cancer may not be captured consistently in adjudicated claims for cervical cancer.
Conclusion
Further research is needed to analyze the breakdown of cervical cancer cases by race and ethnicity to understand any disparities in screening and outcomes. Additionally, researching healthcare resource utilization (HCRU) costs post-diagnosis will help stakeholders understand the cost of not screening per recommendations and how HCRU varies based on the age at which cervical cancer is diagnosed. The 71+ population can also be further studied in Medicare FFS data to understand the impact of limited screening criteria, on the early diagnosis of women in this age group.
Current and additional findings can help inform stakeholders in the primary care, gynecologic, and cervical cancer space. Healthcare providers play an important role in communicating the importance of screening. For payers, the costs associated with treating cervical cancer patients may drive a focus on early screening and access to screening. Manufacturers of cervical cancer diagnosis tests and therapies can identify barriers within the patient journey and partner with providers to ensure early and timely screening and diagnosis. Additional research into demographic factors, age at diagnosis, and long-term costs could further inform screening guidelines, resource allocation, and targeted interventions to address cervical cancer disparities.
How Can Avalere Help?
Stakeholders across the care continuum including providers, payers, patients stand to benefit significantly from a proactive approach to preventive care and early detection. Avalere supports these stakeholder address key questions and initiatives like those identified in this study through:
- Stakeholder primary research can provide insights into stakeholder decision-making motivations and gaps in the care continuum;
- Patient support services guidance can support education and access solutions to overcome barriers to care.
To learn more, connect with us.
Data Source
For this analysis, Avalere used commercial and Managed Medicaid claims data from Inovalon’s proprietary “Medical Outcomes Research for Effectiveness and Economics” (MORE2) Registry®, accessed by Avalere via an Agreement with Inovalon, Inc.
January 23, 11 AM ET
Learn More


