Admissions From EDs Increased for FFS Beneficiaries in 2020
Summary
In 2020, the total number of emergency department (ED) visits for Medicare fee-for-service (FFS) beneficiaries declined, but patients presenting with non-emergency care sensitive conditions were more likely to be admitted than in 2019.Avalere found that, while ED visits for FFS beneficiaries dropped at the start of the COVID-19 pandemic and remained lower than 2019 throughout 2020, the percentage of ED visits that resulted in an inpatient admission was higher in 2020 compared to 2019. This was the case for all visit types but was especially true for conditions that are traditionally non-emergency care sensitive, defined as conditions that tend to be of lower acuity or less time sensitive to treat.
Background
In the spring of 2020, COVID-19 reached pandemic status, and many healthcare facilities closed for non-emergencies. While overall Medicare utilization dropped precipitously at the onset of the COVID-19 pandemic, it mostly bounced back toward the end of 2020. Avalere analyzed ED utilization among Medicare FFS beneficiaries to understand how the pandemic influenced the way this group sought care. Avalere found there were fewer ED visits overall, but beneficiaries who did visit the ED presented with more severe cases, which led to a higher inpatient admission rate.
Emergency Department Visits
Average ED utilization was 20% lower across all of 2020 compared to 2019, with the largest decrease in April 2020 when ED utilization was 46% lower than in 2019. The decrease in ED visits aligned with the first wave of COVID cases in April 2020. Spikes in COVID cases in the summer and winter of 2020 also align with a flattening or decreasing in the rate of ED visits (Figure 1).

Data on new COVID cases in 2020 was from the Centers for Diseases Control’s COVID tracker.
On March 13, 2020, President Trump declared a national emergency.
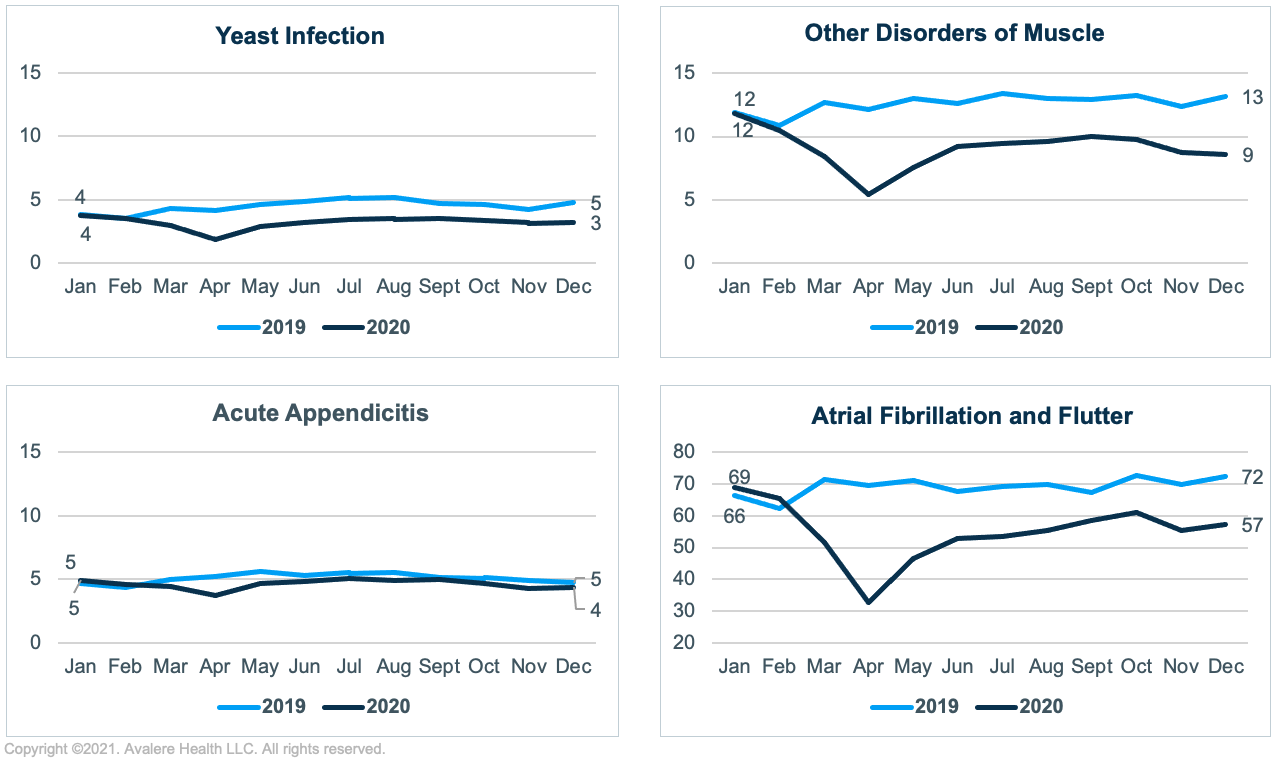
Utilization decreased for conditions that were more sensitive to emergency care such as atrial fibrillation and flutter (International Classification of Diseases–10th rev. [ICD-10], I48) and acute appendicitis (K35), as well as those less sensitive to emergency care such as yeast infection (B37) and other disorders of muscle (M621; Figure 2). Conditions sensitive to emergency care tend to be severe (e.g., morbidity associated with an untreated, perforated appendix—namely sepsis—is high in older adults) or require a rapid response (e.g., delays in correcting cardiac rhythm can lead to a greater risk of stroke).2 Conversely, while treatment for non-emergency care sensitive conditions should occur in a timely manner to avoid adverse events, treatment can often take place outside of the ED (e.g., yeast infections can be treated by a primary care provider). This is not to say that it is never appropriate to use the ED for conditions deemed non-emergency care sensitive, only that on average most cases of these conditions do not require emergency care.
Avalere found the decrease in 2020 ED visits was greater for conditions not as sensitive to emergency care (28% decrease for other disorders of the muscle and 29% decrease for yeast infections) than for emergency care sensitive conditions (21% decrease for atrial fibrillation and flutter and 9% decrease for acute appendicitis), relative to 2019.
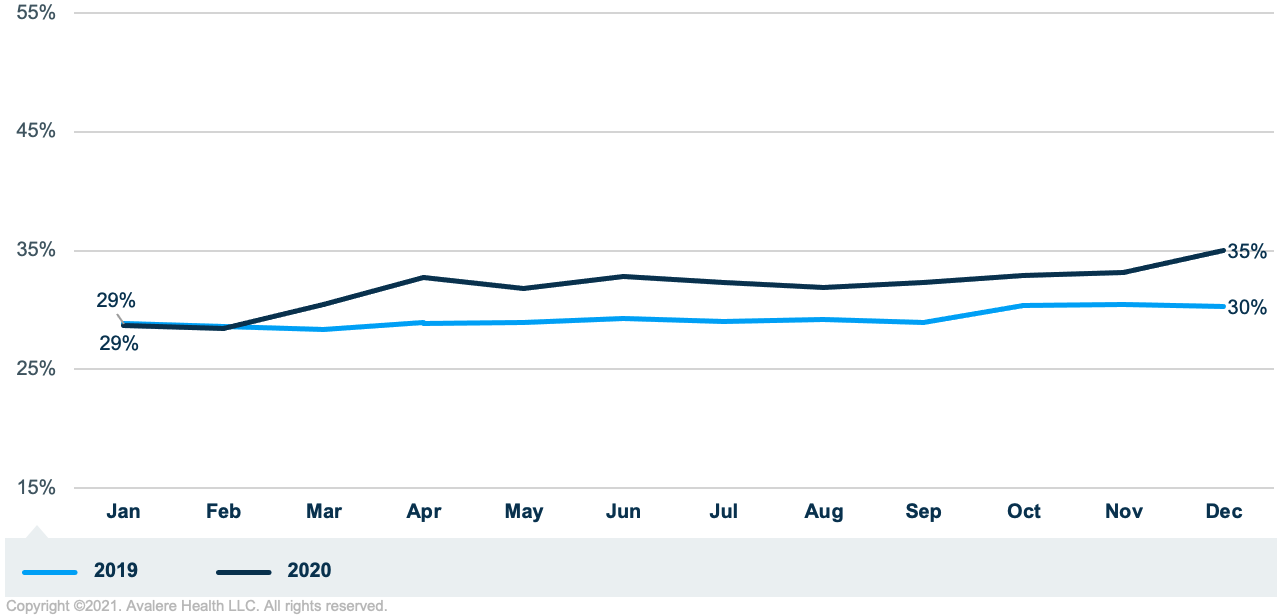
Inpatient Admissions from the ED Utilization Trends
ED visits are classified as outpatient or inpatient depending on whether the patient was admitted to the hospital. Although there were year-over-year decreases in ED visits in 2020 compared to 2019, there was an increase in the percentage of ED visits that resulted in inpatient admissions. The percentage of ED visits resulting in an inpatient admission increased 9% on average for 2020, with the highest increase in April of 2020 (13% increase). For both January and February (pre-pandemic), the difference in admissions from the ED was less than 1% between 2019 and 2020 (Figure 3).
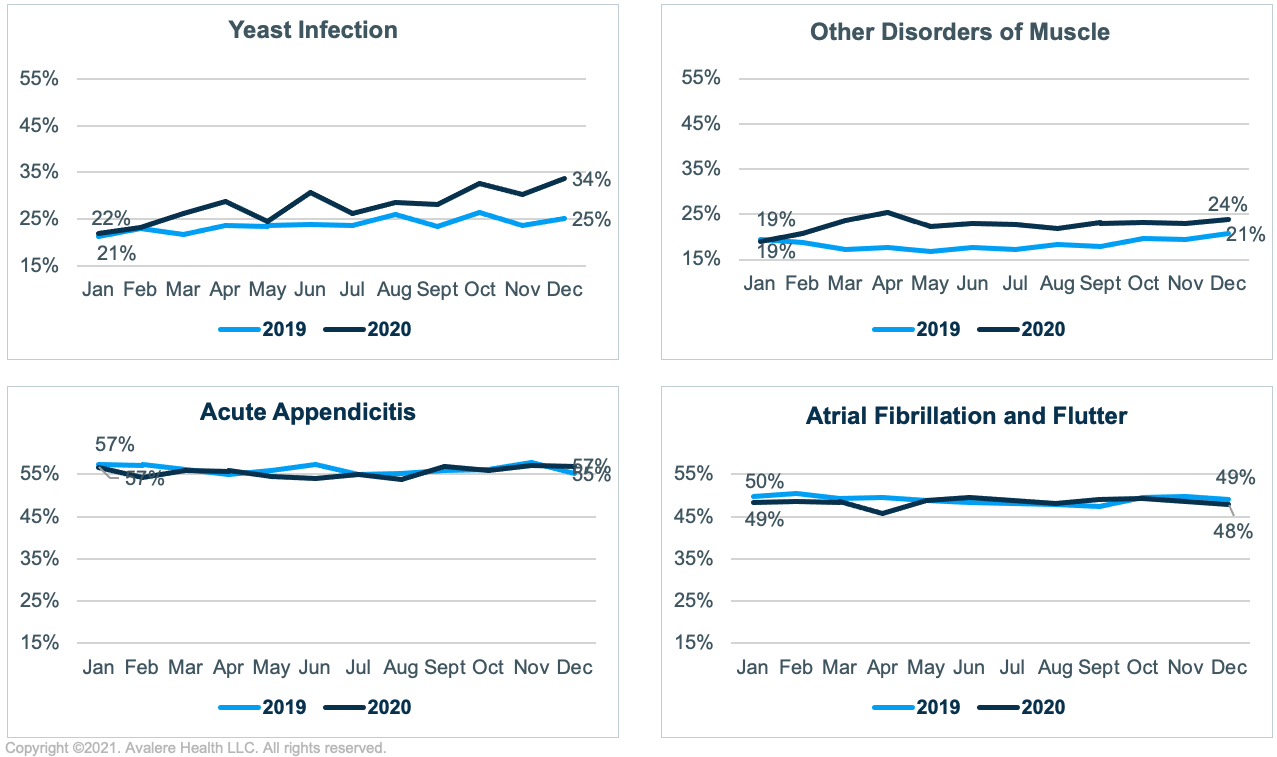
Unlike ED visits, which decreased for almost all conditions,3 the increase in inpatient admissions was mostly confined to non-emergency care sensitive conditions. The average IP admission rate for other disorders of the muscle was 18%in 2019 and 23% in 2020 (28% higher in 2020), and the average inpatient admission rate for yeast infections was 24% in 2019 and 28% in 2020 (17% higher in 2020). For emergency care sensitive conditions, the inpatient admission rate did not follow this trend; on average, there was little change between the 2019 and 2020. Overall, there was a 1% decrease from 2019 to 2020 in average inpatient admission rate for both atrial fibrillation and flutter and acute appendicitis.
Conclusion
For some conditions, the ED is the appropriate site of care and an ED visit is unavoidable. Conversely, the ED is often not the optimal site of care for non-emergency care sensitive conditions. During the pandemic, FFS beneficiaries changed their ED-use behaviors, visiting the ED less for both emergency and non-emergency care sensitive conditions. Although Avalere’s analysis found fewer ED visits overall, beneficiaries often presented with more severe cases when they did go to the ED. This was evidenced by Avalere’s findings that, compared to 2019, 2020 ED visits were lower and inpatient admissions for non-emergency care sensitive conditions relative to all admissions were higher.
The COVID-19 pandemic has affected behaviors and interactions throughout society, including the healthcare sector. Some behaviors observed in 2020 are new, such as decreased use of preventive care and routine immunizations. However, some behavior changes were in motion before 2020 and were accelerated by the pandemic, such as a shift to outpatient care. The policies implemented during the pandemic, such as telehealth parity and relaxing some scope of practice laws, will continue to influence utilization unless repealed or changed when the pandemic subsides. As the COVID-19 pandemic moves to a more endemic scenario, policy makers and industry leaders have an opportunity to be proactive about shaping these behavior changes, which will have ripple effects on future healthcare utilization and health status of the population.
To receive Avalere updates, connect with us.
Methodology
Avalere identified a cohort of Medicare FFS beneficiaries in 2019 and 2020 using the 100% file of Medicare FFS Parts A and B data, accessed via a research-focused data use agreement with the Centers for Medicare & Medicaid Services. Inclusion criteria for each year required 6 months of FFS enrollment in that year and no enrollment in a Medicare Advantage plan in that year. For the ED visit to be included, the beneficiary had to be enrolled in Medicare FFS during the month of the ED visit.
ED diagnosis was identified by ICD-10 codes aggregated to the ICD-10 category level (the first 3 digits of the ICD-10 code). Avalere used the primary condition for the ED visit. Conditions were selected to represent both emergency care sensitive and non-emergency care sensitive conditions. A 2019 study in which the authors queried experts to create a list of emergency care sensitive conditions was used as a reference in identifying conditions.4
Outpatient and inpatient ED visits were defined by revenue center codes 0450, 0451, 0452, 0456, 0459, and 0981 in the inpatient and outpatient Medicare files. Inpatient stays from outpatient ED visits were identified as any inpatient visit that occurred within 3 days of a beneficiary’s outpatient ED visit and where there was the same primary diagnosis code as the outpatient ED visit. Inpatient ED visits and inpatient stays from the outpatient ED visits were summed for total inpatient stays from the ED. Outpatient and inpatient ED visits were summed for total ED visits, and the admission rate was calculated as the number of inpatient stays from the ED over the total number of ED visits.
Notes
- The ICD-10 category for “other disorders of muscle” includes conditions such as nontraumatic muscle separation or rupture, muscle wasting and atrophy, generalized muscle weakness, and muscle spasms.
- Vashi AA, Urech T, Carr B, et al., “Identification of Emergency Care–Sensitive Conditions and Characteristics of Emergency Department Utilization,” JAMA Netw Open 2.8 (2019):e198642. doi:10.1001/jamanetworkopen.2019.8642.
- ED visits for some respiratory conditions were up in the early months of the pandemic compared to the same months of 2019.
- Vashti et al., 2019.





