Medicare FFS Utilization Decreased During the COVID-19 Pandemic
Summary
Avalere analysis finds healthcare utilization among Medicare Fee-for-Service (FFS) beneficiaries decreased in the spring of 2020 compared to the spring of 2019.Background
In the spring of 2020, lockdowns were imposed across the US in order to prevent the spread of COVID-19. During these lockdowns, healthcare facilities were closed for most care, with the exception of acute and emergency services. To examine the impact of COVID-19 lockdowns on healthcare utilization, Avalere assessed Medicare FFS claims volume for hospital inpatient, hospital outpatient, and professional/physician services during the first 6 months of 2020 as compared to the first 6 months of 2019.
Results
Avalere found healthcare utilization decreased in the first 3 months of the pandemic (March, April, and May of 2020) compared to these same months in 2019. This decrease was largest in April when there was a 51% reduction in outpatient claims and a 42% reduction in professional claims in 2020 compared to 2019.

Avalere also examined healthcare utilization changes between the first half of 2019 and 2020 by race and found that utilization among the White Medicare population decreased more than among the Black or Hispanic populations. However, the largest utilization decreases were observed among the Asian beneficiaries, who account for 2% of the overall Medicare FFS population (White Medicare beneficiaries constitute 81%; Black Medicare beneficiaries, 9%; and Hispanic Medicare beneficiaries, 2%; Figure 2).

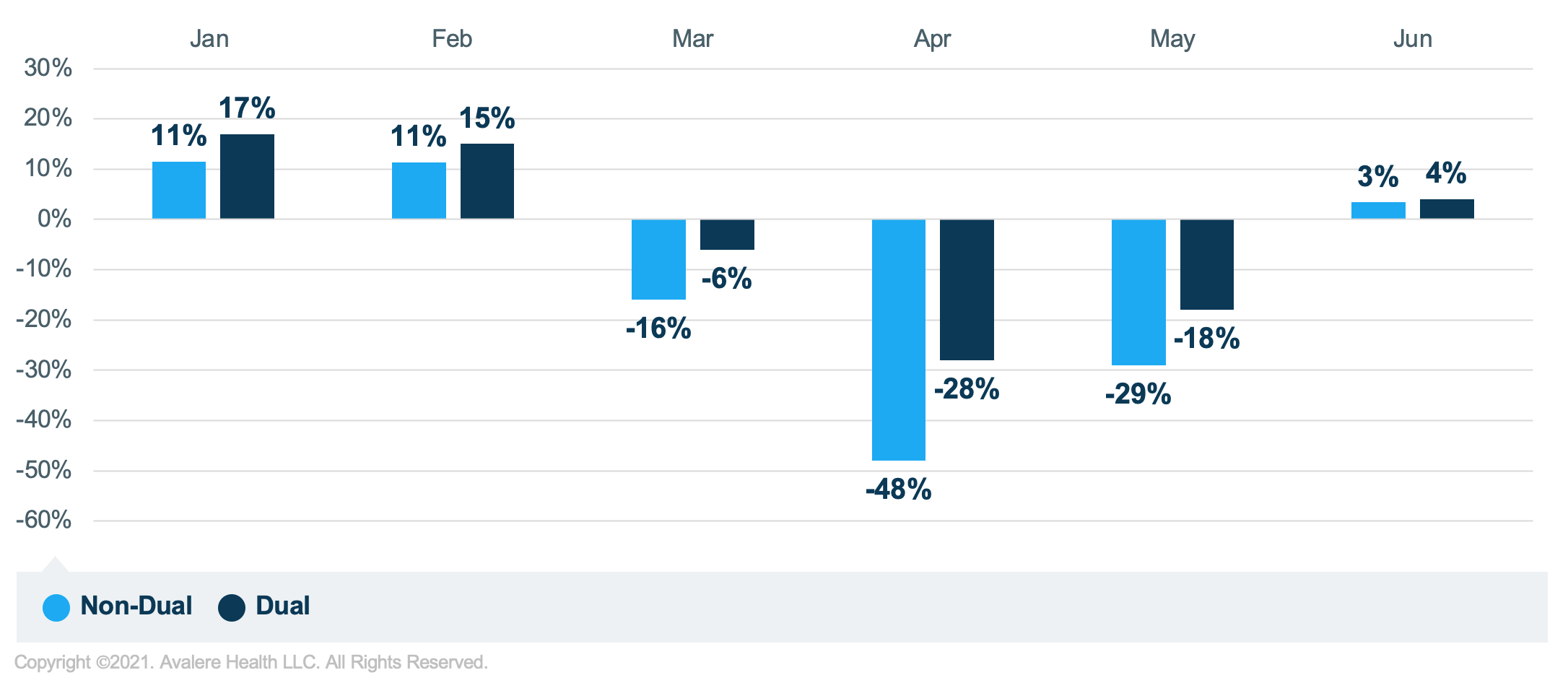
Lastly, Avalere found a larger decrease in claims for non-duals than for the dual-eligible population (Medicare beneficiaries also eligible for Medicaid). While duals and non-duals looked similar in terms of their utilization rates in January and February of 2020 compared to the same months of 2019, the groups deviate in the spring. Dual-eligible beneficiaries had 28 fewer claims in April of 2020 compared to April of 2019, while the number of claims per non-dual eligible Medicare beneficiaries fell 48% in April 2020 compared to April 2019 (Figure 3).
Conclusion
Avalere will continue to monitor the impact of the COVID-19 pandemic on healthcare utilization among Medicare FFS beneficiaries. Additional analyses of the types of services received and forgone could help explain racial and socio-economic differences in the decreases in utilization between 2019 and 2020.
The impact of delayed or avoided care on the health status of Medicare beneficiaries will need to be examined over the following months and years as there could be lasting effects even as the pandemic recedes. In addition, decrease in service utilization could indicate that people missed out on preventive care and postponed care they may have needed to receive, which contributes to compounding concerns in management of chronic and acute care leading to pent up demand in future months in addition to potential healthcare costs associated with gaps in care. Avalere continues to evaluate the potential impact of forgone preventive and maintenance care on beneficiary health status.
To receive Avalere updates, connect with us.
Methodology
To conduct this analysis, Avalere used a 20% random sample of Medicare Part A and Part B FFS claims data obtained under a research data use agreement with the Centers for Medicare and Medicaid Services. All claims with “thru date” (the last day of the billing statement for services) between January 1, 2019, and June 30, 2019, and between January 1, 2020, and June 30, 2020, were included in this analysis. Avalere identified beneficiary enrollment and characteristics using the Master Beneficiary Summary File. For inclusion in the analysis, Avalere required that the enrollee be in Medicare in both 2019 and 2020. Avalere applied this restriction in order to identify how claims changed for a cohort of beneficiaries.






