Opportunities for Savings Within Orthopedic Value-Based Bundles
Summary
It is critical for orthopedic providers to understand key cost drivers to identify opportunities for savings in bundled payment arrangements with private payers.Given the success in generating savings and improving outcomes from Centers for Medicare and Medicaid Innovation Center (CMMI) models such as the Comprehensive Care for Joint Replacement (CJR) model and surgical events in the Bundled Payments for Care Improvement Advanced (BPCI-A) model, there is growing interest in value-based payment arrangements with private payers. Avalere worked with a large orthopedic group to develop a value-based contract (VBC) roadmap and build a flexible model to understand bundle pricing mechanisms and opportunities for savings in orthopedic VBCs with private payers.
To accomplish this, Avalere gathered information on the practice’s existing payer contracts, patient demographics, and market presence. Avalere identified the practice’s Medicare patients who underwent total joint replacements (TJRs) using its 100% Medicare Fee-for-Service (FFS) data, which is a valuable asset for understanding commercial populations where private payer data are limited. This comprehensive data source was risk adjusted based on organization-specific patient demographics of the commercial and Medicare Advantage (MA) populations of interest to understand healthcare usage in the practice’s privately insured patients. Avalere then identified related services (e.g., pre-surgery visits, imaging, anesthesia, post-acute care [PAC] services, physical therapy [PT], surgical complications) provided to these patients between 30 days before surgery and 90 days after surgery.
Methodology
Under a research-focused data use agreement with the CMS, Avalere examined data from CMS’s Medicare Part B FFS claims from February 2019 to March 2021 to identify beneficiaries who received a total joint replacement in the practice’s service area during that period. Avalere identified beneficiaries with the following Current Procedural Terminology codes: 27130, 27132, 27447, and 23472. Avalere used the Prometheus Episode grouper code sets for total hip replacement (THR), total knee replacement (TKR), and total shoulder replacement (TSR) to identify healthcare services associated with the total joint replacement procedures provided to these patients. Avalere emulated the Maryland Episode Quality Improvement Program (EQIP) episode structure and identified episodes of care from 30 days before surgery and 90 days after surgery. Avalere validated episode costs identified in our model by comparing these to the existing EQIP target prices for the practice of interest.
Avalere developed a sophisticated and flexible model to simulate practice profitability over 3 years in multiple commercial and MA VBC arrangements for TJRs using inputs such as membership numbers by line of business, medical inflation for future projections, site of service, patient demographics, services included in the bundle price, adjustments to account for surgical complications, and practice expenses. The resulting tool calculated bundle price changes based on the user-driven inputs to inform the practice’s VBC contracting decisions. Avalere delivered the model and corresponding model orientation to the client to support its use for contracting decisions. Figure 1 is a sample of the model orientation presentation.
Key Considerations for Orthopedic Practices
The Avalere analysis yielded multiple key learnings about opportunities for savings in orthopedic VBCs:
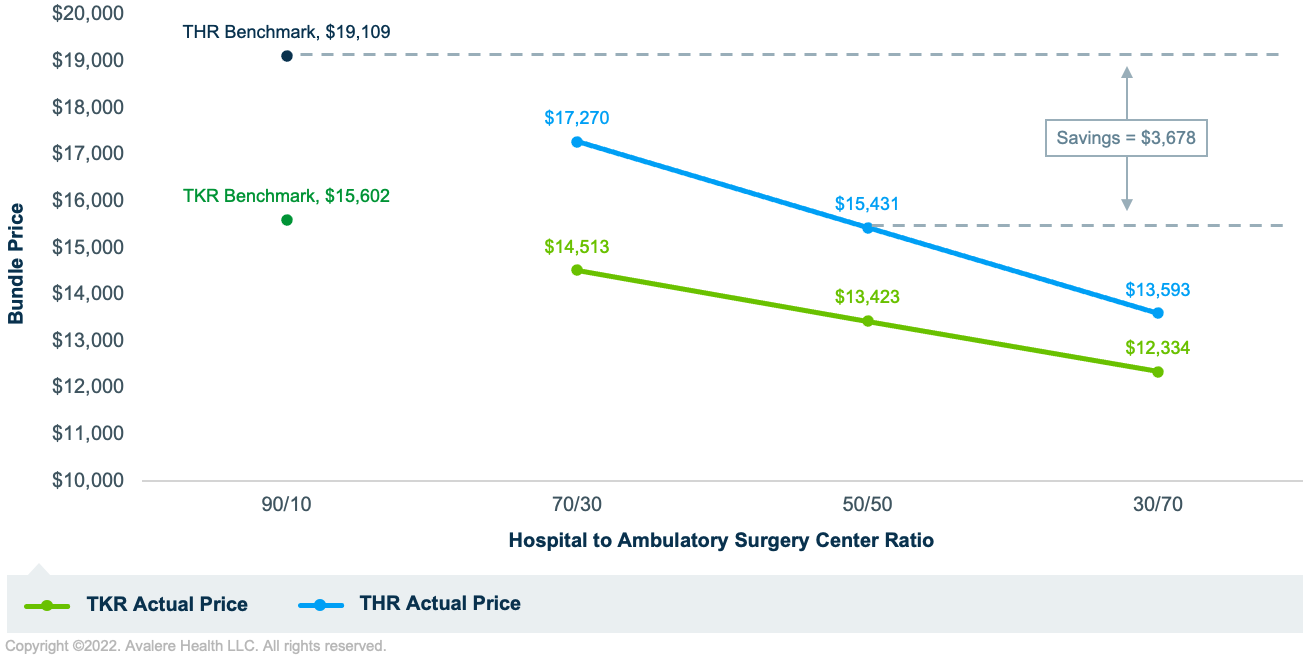
Shifting the site of care from the inpatient to the outpatient setting resulted in the largest TJR bundle price difference.
- In a same-day bundle for Medicare patients in the orthopedic practice of interest, shifting the ratio of THRs in an ambulatory surgery center (ASC) from 10% to 50% results in a price reduction of more than $3,500 per THR. (See Figure 2 below for the impact of site of service shifts on TKR and THR episode revenue in the Medicare population.)
Additional opportunities for savings lie with shifting PAC services away from the inpatient setting and reducing PT costs.
- Including PAC and PT costs in a THR bundle add around $1,000 and $700 to each bundle price, respectively.
- Practices may contract with innovative digital health companies to reduce costs by providing PAC and PT services at home, while maintaining quality of care and patient engagement to prevent costly readmissions and adverse outcomes.
Another important conclusion from Avalere’s analysis is the significance of the benchmark and bundle inclusion criteria. It is important for orthopedic practices entering into VBCs to consider implications of different benchmark-setting methodologies on their success. For example, a low-cost provider in the region may want to set their benchmark price based on their regional competitors’ prices rather than their own historical performance to prevent competing against themselves in a so-called “race to the bottom.” Additionally, a practice should consider where they have room for improvement and cost savings to determine what services are included in a bundle price, as well as the specific patient demographics and utilization patterns for a certain payer when going into contract negotiations
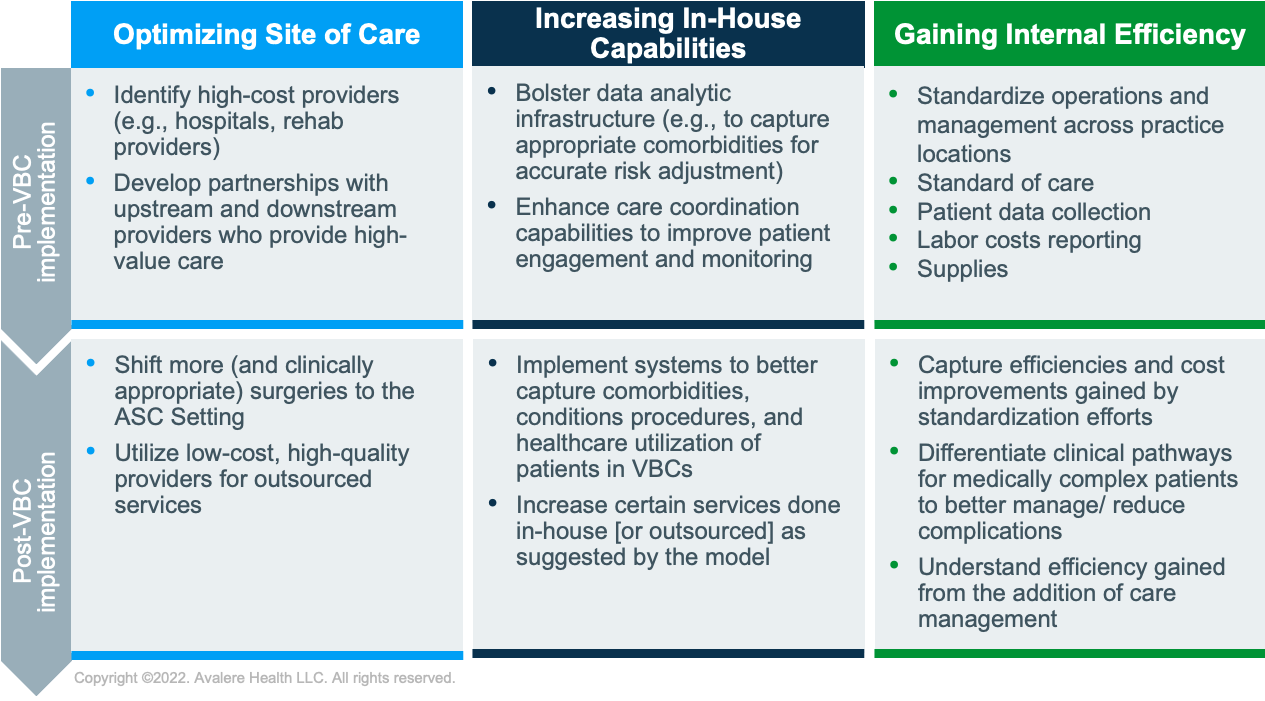
Orthopedic practices can utilize models built on claims data to simulate VBC performance by comparing a benchmark price of a certain VBC bundle to the potential bundle price with forecasted changes to site of service, PAC costs, and gained efficiencies, among others. The difference between the benchmark and the modeled bundle price represents the savings—or potentially losses—realized by the practice given the modeled changes. This activity informs the most impactful changes a practice can make to improve performance in a VBC. Figure 3 provides a framework for potential actions a practice can take to realize success in VBCs, which may be applied to other surgical specialties in the future.
Next Steps and Looking Forward
TJRs are seen as a key cost driver for orthopedics, and existing CMMI models such as BPCI-A and CJR can inform bundle-based VBC design and execution with private payers. However, bundle based VBCs do not account for the majority of an orthopedic practice’s business. After gaining experience and building capabilities in bundled VBCs, orthopedic practices may consider creating a capitated per-member-per-month model for all musculoskeletal care delivered to patients, beyond just TJR procedures.
For practices looking to perform a similar exercise to the model Avalere developed, it is important to modify underlying claims data to follow a single archetype. Once this underlying data is consistent, the model is powered to be flexible to adapt to different population demographics, payers, and geographies. A flexible model is key to accurately identifying cost drivers and opportunities for savings in value-based arrangements.
To keep up with the latest changes to CMMI models, connect with us.







