
Federal and State Policy
As the largest US healthcare payer, the federal government plays a dominant role in shaping the healthcare marketplace, while states take center stage when it comes to developing novel policy approaches. Our experts track, interpret, and model policies that affect insurance coverage, access, and consumer choice so you can see around the bend.

CMS Methodology for Calculating Payment Errors May Result in Underpayments to Health Plans
In February 2012, the Centers for Medicare & Medicaid Services (CMS) announced a final payment error calculation methodology for its contract-level Risk-Adjustment Data Validation (RADV) audits of Medicare Advantage (MA) plans.
State-Run Reinsurance Programs Reduce ACA Premiums by 19.9% on Average
New analysis from Avalere finds that states with their own reinsurance programs reduce individual market premiums by 19.9% on average in their first year.

Top 4 Steps to Ensure Operational Readiness for RAPS to EDS Transition
As CMS continues to transition from the Risk Adjustment Processing System (RAPS) to the Encounter Data System (EDS) for Medicare Advantage (MA) risk score calculation, plans must evaluate operations and close gaps to minimize the impact of risk score differences using this claims data source.
Effect of Potential Policy Change to Part D Generic Tiering on Patient Cost Sharing and Part D Plan Costs
In a new analysis, Avalere examines the implications of CMS’ potential new requirement that Part D plans place generics only on generic tiers.
Uses and Limitations of Medicare Advantage Encounter Data
In a recent post on the Health Affairs Blog, we examine the potential uses and limitations of Medicare Advantage (MA) encounter data.
HHS Proposed Changes Could Reduce ACA Coverage and Increase Premiums
New analysis from Avalere finds that exchange plan sign-ups could decline by 1.1 million, while premiums could increase by 6.3%, by 2025 should HHS finalize recently proposed changes to auto-reenrollment in the exchange and the calculation of tax credit subsidies.
Avalere Welcomes Jason Altmire as Senior Advisor
Former U.S. Congressman Jason Altmire has joined Avalere Health as a senior advisor, offering his deep understanding of the policy-making process to inform business strategy.
CMS Highlights Potential Changes that Could Restrict Access to and Increase the Costs of Certain Brand Drugs to Obamacare Enrollees
The Centers for Medicare & Medicaid Services released the proposed Notice of Benefit and Payment Parameters (NBPP) for the 2020 plan year. The rule could limit exchange plan enrollees' access to certain brand name drugs and increase the out-of-pocket costs within plans.
Interview: Key Takeaways on the Ruling Declaring the Affordable Care Act Unconstitutional
Avalere experts discuss the implications for a recent decision ruling the Affordable Care Act is Unconstitutional.
New HRA Rule Could Reshape Enrollment and Access in Individual and Employer Markets
A proposed rule released by the Treasury Department, Department of Labor, and Department of Health and Human Services would expand the allowed uses of employer-sponsored Health Reimbursement Arrangements (HRA). Comments on the rule can be submitted until December 28, 2018.

Free Exchange Plan Options Are Available in Most Counties for 2019
New analysis from Avalere finds that over 95% of counties with exchanges operated by HealthCare.gov have free plan options for low-income consumers.

Health Plans with More Restrictive Provider Networks Continue to Dominate the Exchange Market
Narrow network plans comprise nearly three-quarters of the exchange market.
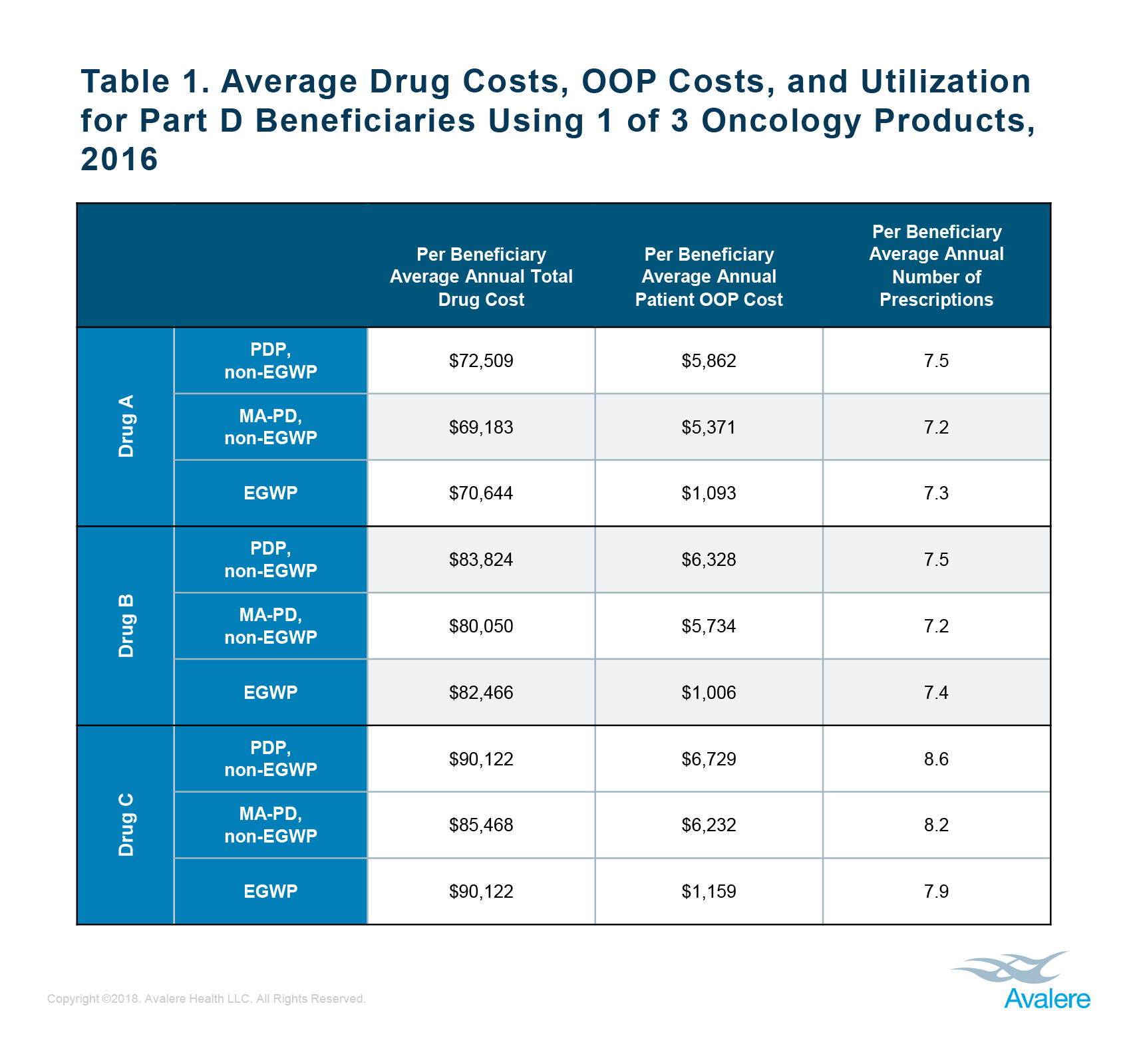
Out-of-Pocket Costs for Oncology Drugs Vary Substantially Between Employer and Non-Employer Based Part D Plans
New Avalere analysis finds that beneficiaries enrolled in Employer Group Waiver Plans (EGWPs) have lower out-of-pocket (OOP) costs for select drugs than beneficiaries enrolled in other types of Part D plans.
Interview: E3 – Trends in Health Policy and the Mid-Term Elections Results
In the last interview of our mid-term elections series, Avalere experts Chris Sloan and Elizabeth Carpenter discuss potential implications on health policy.

New Opioid Law Takes Broad Aim at Opioid Crisis
The Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act, signed into law on October 24, 2018, takes aim at the opioid crisis from multiple angles.
Interview: E2 – Key Mid-Term Elections Driving Medicaid Expansion to Watch
Avalere experts, Chris Sloan and Tiernan Meyer, discuss potential state and federal-level scenarios for Medicaid expansion.
Interview: E1 – Impacts the Mid-Term Elections Could Have on Pre-Existing Conditions
In the first interview in our 3-part series covering the mid-term elections and potential implications on health policy, Avalere expert Chris Sloan explores potential implications of the mid-term elections on health policy. To kick off the series, Avalere Founder, Dan Mendelson, discusses pre-existing conditions.

Access to Abuse-Deterrent Opioid Formulations Tied to Reduced Risk of Opioid Abuse and Overdose
New Avalere research finds that health plan members enrolled in plans that cover abuse-deterrent formulations (ADFs) of opioids have a lower risk of opioid abuse (OA) and overdose (OD) and lower opioid abuse-related hospitalizations than people in plans that do not offer coverage of ADF opioids.

Trends in Opioid Use: History, Background, and Origins of the Epidemic
Shift in clinical practice as far back as 30 years ago planted the seeds for the current opioid epidemic. New research by Avalere Health finds that between the mid-1980s and 1990s, individual pharmaceutical manufacturers, national scientific bodies, and professional societies began a push to treat pain more aggressively.

2.7 Million People Could Gain Access to Medicaid Coverage Based on Outlook for State Elections
New analysis from Avalere finds that 2.7 million individuals from states that have not expanded Medicaid could gain Medicaid coverage should their newly elected governors decide to expand the program or states pass expansion referenda on their ballots.


