
Federal and State Policy
As the largest US healthcare payer, the federal government plays a dominant role in shaping the healthcare marketplace, while states take center stage when it comes to developing novel policy approaches. Our experts track, interpret, and model policies that affect insurance coverage, access, and consumer choice so you can see around the bend.


Patient Out-of-Pocket Assistance in Medicare Part D: Direct and Indirect Healthcare Savings
Avalere examines the effect of foundation-sponsored financial assistance on out-of-pocket costs and federal spending.

Policymakers Seek to Balance Patient Information Sharing with Privacy Protections
Coordinated information sharing can facilitate the delivery of integrated care to patients using both physical and behavioral health services.
Limits on Opioid Prescriptions Are Becoming More Widespread
In response to the concern that overprescribing is a driver of the opioid crisis, payers are limiting opioid fills as one solution.
CMS Gives More Flexibility to States When Regulating Health Insurance
The Centers for Medicare & Medicaid Services released the final Notice of Benefit and Payment Parameters (NBPP) for the 2019 plan year.

Adapting to Medicaid Changes and Trends in 2018
On March 6, Avalere experts came together to discuss the latest Medicaid developments.

Medicare Patients Are Using Fewer Skilled Nursing Services
New research from Avalere finds Medicare beneficiaries are spending fewer days in skilled nursing facilities (SNFs) since 2009 on a per capita basis.

Webinar: Medicaid: Adapt to the Changes
Avalere experts discuss an evolving Medicaid program supported by a new administration and novel state approaches.

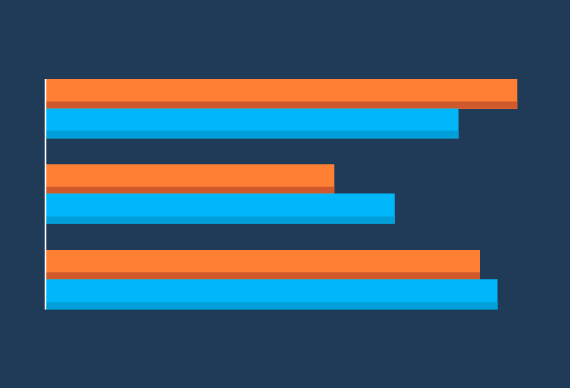
Association Health Plans Projected to Enroll 3.2 Million Individuals
New analysis from Avalere finds that the proposed rule on association health plans (AHPs) is projected to lead to 3.2M enrollees shifting out of the Affordable Care Act's (ACA) individual and small group markets into AHPs by 2022.

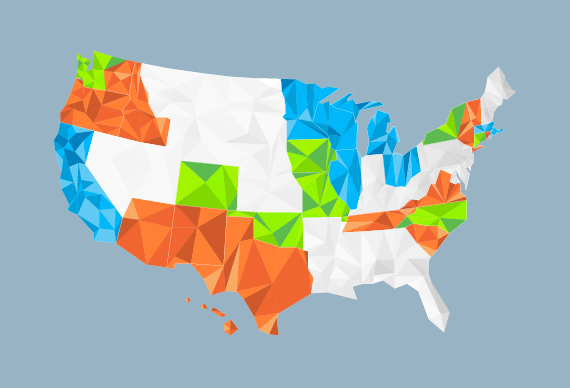
Midwest and Mid-Atlantic States Face Provider Shortage to Address Opioid Epidemic
New research from Avalere Health finds 11 states and DC lack an adequate number of providers certified to prescribe buprenorphine, a medicine used to prevent relapse in people with opioid dependence.
Congress’ 2018 Budget Includes Updates for Providers
On February 9, the Senate voted to pass the Bipartisan Budget Act of 2018, which funds the government through March 23, lifts spending caps for 2 years, and suspends the debt ceiling until March 2019.

Our Take on the President’s FY2019 Budget Proposal
Today, the Trump Administration released its budget for fiscal year 2019 (FY 2019).

Impact of Coverage Gap Discount Changes in Budget Agreement
Avalere experts provide their insights on what the impact of coverage gap discount changes in budget agreement.

Our Take on the 2019 Advance Notice and Draft Call Letter
Yesterday, the Centers for Medicare & Medicaid Services (CMS) released Part II of the Advance Notice and Call Letter (ANCL), describing the Agency's proposed 2019 payment policies and other policy updates for the upcoming plan year for Medicare Advantage (MA) and Part D plans.

Avalere Analysis Shows that Health Needs and Cost of Medicaid Expansion Populations Grow over Time
Beneficiaries show signs of pent-up demand with acute healthcare needs early in their enrollment, but over time costs increase substantially and shift toward chronic care.

What Are Association Health Plans?
On January 4, the Department of Labor (DOL) issued a proposed rule to allow certain self-employed individuals, small businesses, and large businesses, including as part of a professional/trade organization or chamber of commerce, to band together to provide health insurance for their employees and their dependents.
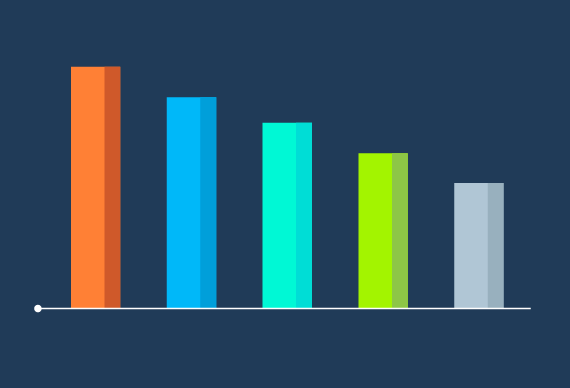
Final 2018 Exchange Enrollment Numbers
At 100% of the OEP, we are at 96% of total Healthcare.gov enrollment compared to 2017 (8.8M n 2018 compared to 9.2M in 2017).

Avalere Develops Report on Opioid Analgesic Trends
Resource presents trends in opioid painkiller prescriptions and deaths due to misuse and abuse.

California, North Carolina, and New York Will See the Largest Provider Payment Cuts and Beneficiary Savings Due to 340B Program Changes
Analysis also finds that 62% of impacted facilities will experience less than a 5% reduction in Medicare Part B revenue due to the drug cuts, but 6% of applicable hospitals will experience cuts greater than 10%.
Funding Reinsurance and Cost-Sharing Reductions Would Lower Individual Market Premiums and Increase Enrollment
New analysis by Avalere examines the impact of two market stabilization proposals-funding the cost-sharing reductions (CSRs) and implementing a federal reinsurance program-on individual market premiums and enrollment.

Plans with More Restrictive Networks Comprise 73% of Exchange Market
Deductibles remain high, nearing $4,000 on average for silver plans.





