More than Half of Health Plans Use Outcomes-Based Contracts
Summary
Cost savings and improved clinical outcomes cited as top advantages for payers according to survey conducted by Avalere Health.New Avalere research finds that 59% of payers have executed an outcomes-based contract (OBC). This type of contracting structure is an agreement between a health plan and drug and device manufacturers that ties product reimbursement to clinical, quality, utilization, or financial outcomes. When Avalere first conducted this survey in 2017, 24% of health plans had an OBC in place.
Thirty-one percent of health plans reported having more than 5 OBCs. In 2017, this number was 12%. Additionally, 21% of payers had 2 to 5 OBCs in place, indicating a 17% increase from 2017.
“Over time, we’ve seen a greater willingness from both health plans and life sciences companies to pursue and execute outcomes-based contracts – clearly something is working, given the continued growth of these types of agreements,” said Sarah Donovan, Head of Client Solutions, Marketing, and Operations at Avalere. “Outcomes-based contracts can provide payers and life sciences companies with an innovative and effective approach to pursue high-value care that is ultimately beneficial for patients.”
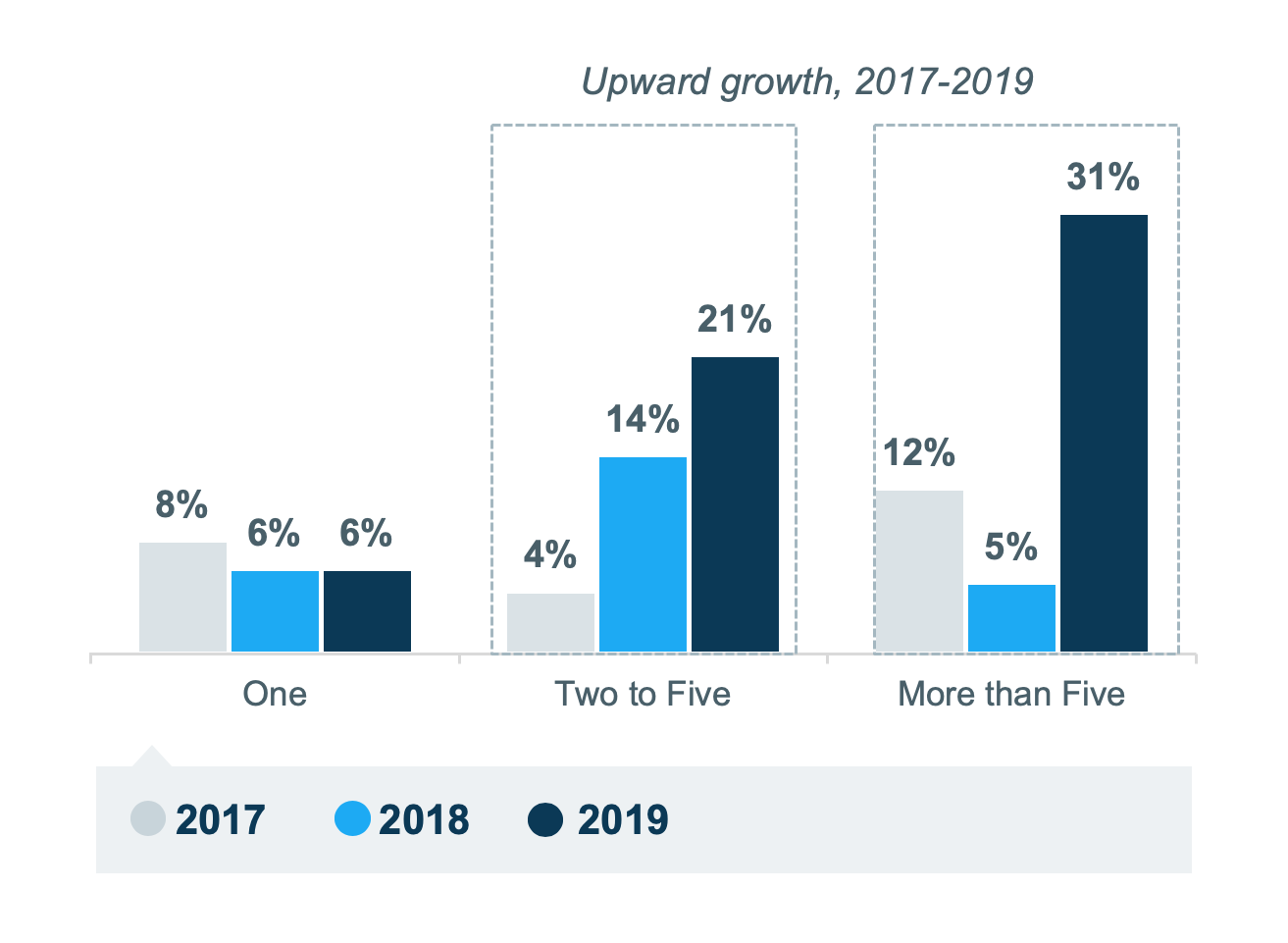 Figure 1. Number of OBCs in Place
Figure 1. Number of OBCs in PlaceAvalere’s survey also found that nearly 60% of health plans with an OBC already in place cited cost savings and clinical improvement as the top advantages of OBCs. Both of these rates have increased since the survey was first conducted in 2017. The capture of real-world information and improved payer–manufacturer relationships were also notable areas of growth.
 Figure 2: Experienced Advantages to Date with OBCs
Figure 2: Experienced Advantages to Date with OBCs“As payers continue to gain greater experience with outcomes-based contracts, their design and measurement of these contracts are becoming more refined and efficient,” said John E. Linnehan, Practice Director, Health Economics & Advanced Analytics. “Outcomes-based contracts have translated into improved cost savings and patient outcomes.”
Avalere’s survey also examined the perceived challenges with OBCs, considerations for looking at a new/existing product, therapeutic areas of focus, cost savings expectations timeline, usage of ancillary services, methods used to measure value, and financial incentives used to execute OBCs.
Avalere will be presenting findings from the survey on October 3 at CBI’s Outcomes-Based Agreements and Innovative Payer Contracting summit in Philadelphia, PA.
Methodology
Avalere conducted a 43-question survey of health plans and pharmacy benefits managers (PBMs) in the United States. The survey was conducted between July 19, 2019 and August 5, 2019 using an online platform for collecting responses. Avalere designed the survey to better gauge and measure current awareness, use, experience, and attitudes toward outcomes-based contracting. Respondents were recruited from a comprehensive panel of health plan and PBM representatives and then screened to determine eligibility. A total of 50 qualified payers participated in the survey.
To receive Avalere updates, connect with us.
Find out the top 2020 healthcare trends to watch.







