Understanding Success Among OCM Participants
Summary
Avalere analysis finds that success in the first 4 performance periods of the Oncology Care Model (OCM) was correlated with reductions to inpatient expenditure and spend reductions within certain high-cost tumor types. Further, smaller community-based practices and those that had lower per-episode expenditure in the baseline period tended to be more successful.The OCM is a voluntary, episode-based payment model developed by the Center for Medicare & Medicaid Innovation (CMMI). The model encourages participating practices to reduce total cost of care and improve care coordination for cancer treatment. In addition to traditional fee-for-service (FFS) payments, participants may bill a $160 monthly enhanced oncology services fee to support care transformation. Participants may also receive a performance-based payment (PBP) if their total expenditures are below a set spending target during a 6-month performance period.
Recent conversations on the efficacy of CMMI’s payment demonstrations and CMMI’s release of the OCM Performance Period 1–3 Evaluation Report has prompted participants and other stakeholders to reflect on what characteristics and behaviors enable practices to achieve success in the model. Many OCM participants report implementing efforts to improve patient navigation, education and outreach, and care coordination. Additionally, practice managers have cited a need to optimize care and reduce expenditure across all aspects of their practice to earn a PBP. To better understand these dynamics, Avalere conducted an analysis comparing attributes of “high-performing” practices to all other participants. Based on available data, Avalere’s analysis focused on the first 4 performance periods (PPs) of the model (episodes initiated July 2016–June 2018) and baseline period prior to the model (January 2012–December 2014).
For the purpose of this study, Avalere identified a subset of practices considered “high-performing,” defined as those estimated to earn 2 or more PBPs in the first 4 PPs of the model. This cohort represented approximately 40% of OCM participants active in PP4. For comparison, Avalere examined all “other” participants along with a matched comparison group of similar nonparticipating oncology practices.
Avalere evaluated how practices’ actual expenditure compared to estimated amounts developed using CMMI’s OCM prediction model. Notably, “high-performing” practices started the model with actual costs that were already lower than CMMI’s predicted amounts. Therefore, these practices were less likely to need to implement significant changes to achieve a PBP. In comparison, the “other” participants began the model with actual expenditure amounts exceeding predicted costs, which did not improve, on average, over the periods analyzed. Overall, this suggests that differences in practice performance may be heavily dependent on expenditure patterns seen prior to the initiation of OCM, thus better positioning some participants for early success.
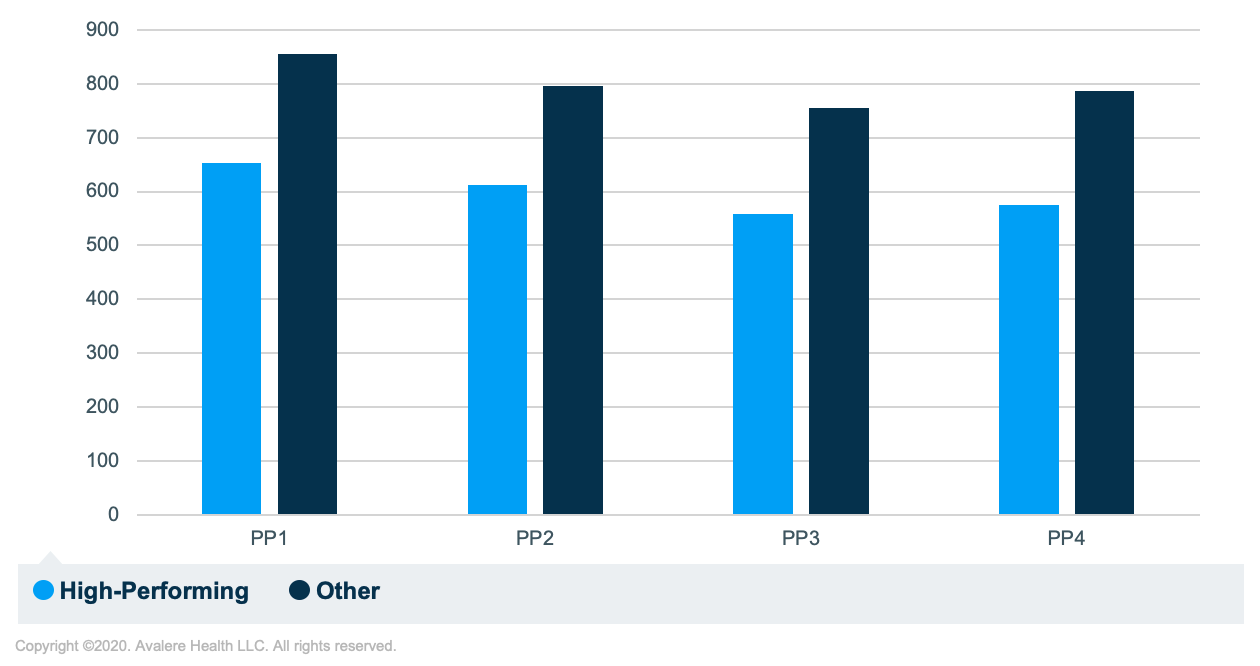
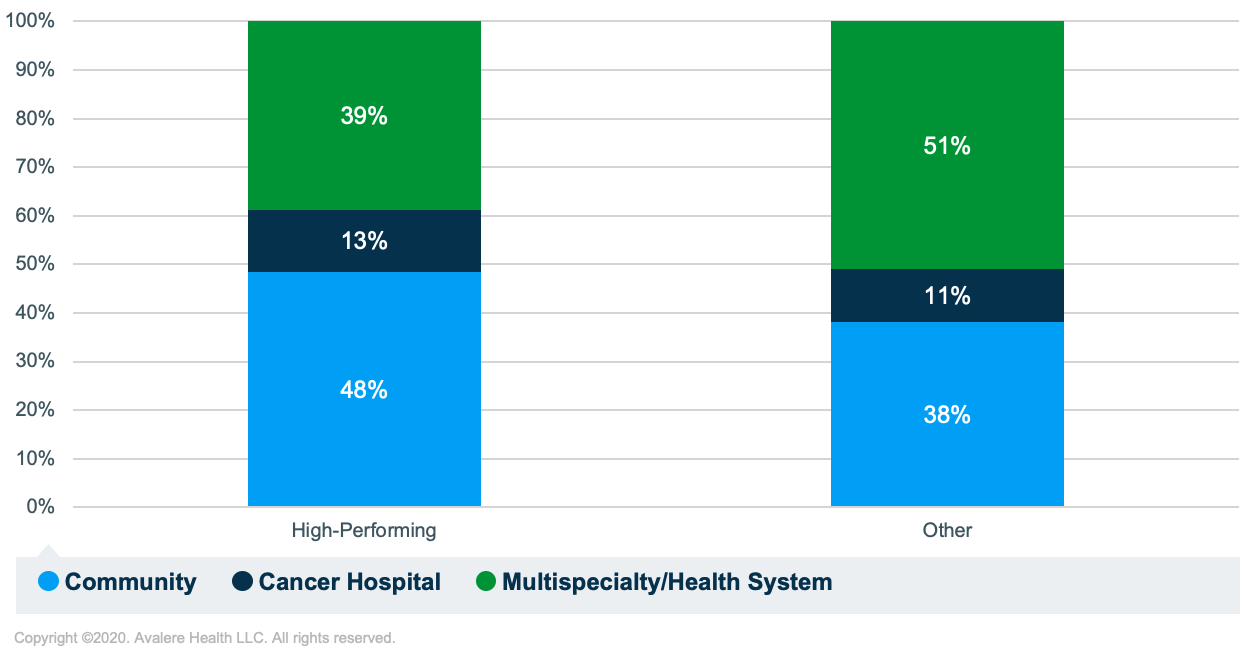
On average, “high-performing” OCM participants had a smaller number of episodes each PP compared to “other” practices. (Figure 1). They also tended to be community-based oncology practices versus multispecialty hospitals (Figure 2). While larger practices benefit from economies of scale and may be better equipped to meet operational demands of OCM, smaller practices can change culture, policies, and behavior to implement change faster and likely have tighter control over expenditure patterns.
The proportion of episodes by tumor type was similar between practice types, suggesting that case mix is not a substantial factor in determining practice success in OCM.
In addition to assessing characteristics of “high-performing” practices, Avalere also examined differences in expenditure patterns. Avalere assessed patterns among “high-performing” practices relative to a comparison group of similar nonparticipants and among all other practices relative to a separate comparison group of similar nonparticipants.
Avalere found that, relative to similar non-participants, “high-performing” practices reduced inpatient expenditure between the baseline period and PP4 by 10% of the OCM baseline average (p-value = 0.097). This change was driven primarily by a reduction in inpatient costs among episodes mapped to a group of OCM hematologic cancer types (i.e., acute leukemia, chronic leukemia, lymphoma, and myelodysplastic syndrome), which represents a 19.5% reduction relative to the baseline average (p-value = 0.070). There was no statistically significant impact on inpatient spend among “other” practices, relative to the comparison group of nonparticipants. Overall, this suggests that practices’ focus on patient navigation to avoid unnecessary hospital admissions may be an effective strategy to reduce the total cost of care.
Finally, Avalere assessed total expenditure within specific tumor types. “High-performing” practices significantly decreased total expenditure across episodes mapped to lung cancer (5.5% reduction relative to baseline average; p-value= 0.066) and high-risk prostate cancer (8.5% reduction relation to baseline average; p = 0.019), relative to their comparison group of nonparticipants. “Other” participants, however, did not exhibit any statistically significant reductions in cost across any of the tumor types evaluated. This suggests that prioritizing reduction in expenditure among high-cost tumor types may also be correlated with success in the model.
While the implementation of the Oncology Care First (OCF) model, the announced successor to OCM, has been delayed due to the COVID-19 public health emergency, many practices are still seeking to understand their own performance and likelihood of success in the future of oncology-focused value-based payment. As of PP8, approximately 90% of practices in the “high-performing” cohort are still participating in the OCM, compared to about 75% of “other” practices. As announced in CMMI’s Request for Information, the OCF model may require OCM practices to take on downside risk immediately, which could deter participation among practices without a clear understanding of how to achieve success in the model. Additionally, practices are uncertain how the proposed Monthly Prospective Payment under OCF would be implemented and how it may impact performance evaluation. Avalere’s evaluation of OCM by practice performance cohort shows a differential impact that is not observed when all participants are evaluated together. These results align with practices’ sustained efforts to reduce inpatient admissions and increase outreach to high-risk beneficiaries. Understanding the factors that enable a practice to be successful in these models, such as reduction of inpatient expenditure and focus on high-cost tumor types, will help strengthen practices’ ability to participate and support the growth of value-based payment in oncology.
Funding for this research was provided by Amgen. Avalere retained full editorial control.
To receive Avalere updates, connect with us.
Methodology
Avalere performed this analysis using Medicare Part A/B FFS claims and Part D prescription drug event data under a Centers for Medicare and Medicaid Services (CMS) research data use agreement. All OCM-eligible Medicare FFS cancer patients receiving cancer treatment were included, which represented less than 20% of total Medicare beneficiaries. Avalere replicated the OCM payment method developed by CMS, including the attribution of episodes to practices, the calculation of participants’ benchmarks, and the estimation of their performance-based payments. Participants were identified in the claims data through tax identification numbers (TIN) reported on Part B claims. Avalere identified 164 practices that were ever enrolled in the OCM through TIN mapping and knowledge of OCM participants. The baseline-period aligns with CMS methodology (January 2012 through December 2014) and the intervention period includes episodes initiated between PP1 and PP4. Intervention episodes were initiated between July 1, 2016, and June 30, 2018, and ended by December 31, 2018.
All OCM participants identified in Avalere’s replicated model were assigned to 1 of 2 cohorts. “High-performing practices” were estimated to have earned 2 or more PBPs between PP1 and PP4, and “other practices” were those estimated to have earned fewer than 2 PBPs in the same period. Each OCM participant was matched with 10 nonparticipants using the following baseline characteristics: episode count, geographic region, place of service for evaluation and management visits, OCM cancer bundle mix, and patient gender distribution, average age, Part D/LIS status, and Hierarchical Condition Category (HHC) coding.
Avalere compared “high-performing” and “other” practices to each other to identify differences between the participant groups. Next, Avalere conducted difference-in-difference (DID) analyses to estimate the impact of OCM among all participants and stratified by “high-performing” and “other” cohorts. The baseline period and intervention periods align with those described above. The DID used a mixed effects model specified at the practice level and controlled for confounding effects, including practice size, average number of HCCs, and facility/office share (from place of service). Individual regressions were run at the tumor type and tumor type/product level, and therefore the DID model did not need to control for tumor type.
January 23, 11 AM ET
Learn More



