News
Graham-Cassidy-Heller-Johnson Bill Would Reduce Medicaid Funds to States by $713B Over the Next 10 Years
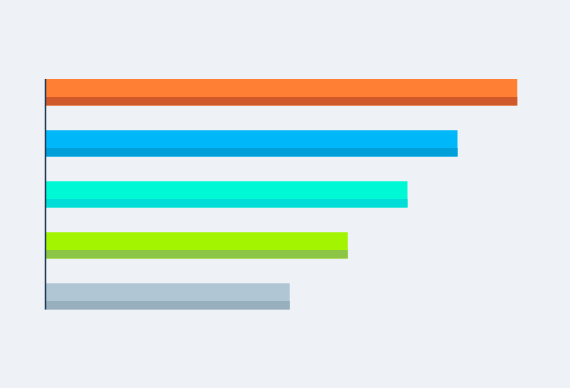
New analysis from Avalere finds that the Graham-Cassidy-Heller-Johnson (GCHJ) bill to repeal and replace the Affordable Care Act (ACA) would lead to a substantial reduction in federal Medicaid funding to states of $713B through 2026 and more than $3.5T over a 20-year period if block grant funding is not reauthorized (Figure 1).
Graham-Cassidy-Heller-Johnson Bill Would Reduce Federal Funding to States by $215B
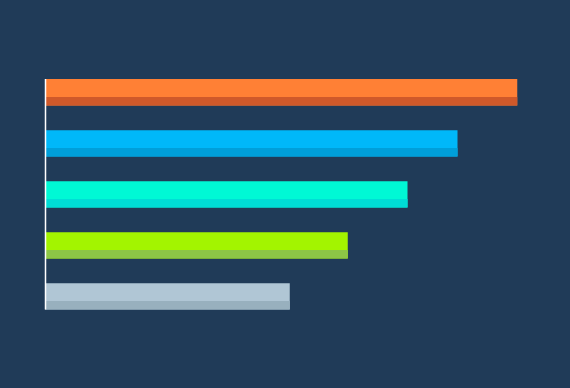
New analysis from Avalere finds that the Graham-Cassidy-Heller-Johnson (GCHJ) bill to repeal and replace the Affordable Care Act (ACA) would lead to a reduction in federal funding to states by $215B through 2026 and more than $4T over a 20-year period (Table 1).

Exchange Reinsurance Stabilization Package Could Reduce 2018 Premiums by 17%
Market stabilization efforts could also lead to higher enrollment in exchanges.

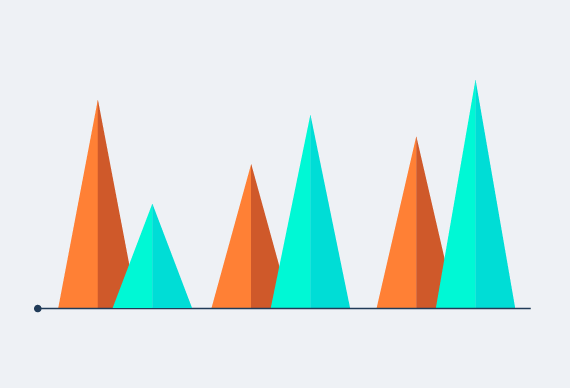
Exchange Plans in Counties with the Least Insurer Competition Have the Highest Premiums
Benefit designs do not vary widely based on insurer competition, except for deductibles that are lower in areas with three or more insurers.

Cruz Amendment to BCRA Would Lead to Coverage Losses and Increased Premiums for Individuals with Higher Medical Expense
Affordable Care Act-compliant plan market would see 39% higher premiums, while non–ACA-compliant plans would have much lower premiums
New Medicare Incentives Encourage Accountable Care Organizations To Assume Greater Risk
Avalere simulation finds that more ACOs will be eligible for earnings if they take on two-sided risk.
Biosimilars Gain Widespread Adoption by Health Plans
New research from Avalere finds that most health plans are covering at least one of the two biosimilar products currently on the market.

Senate Health Bill to Reduce Federal Medicaid Funding to States
New analysis from Avalere finds that states could see federal funding for their Medicaid programs decline by between 6% and 26% under the Better Care Reconciliation Act (BCRA) by 2026.

Premium Increases and Fewer Insurers Participating Expected in Exchange Market in 2018
More than 40% of counties could see only one exchange plan in 2018, with risk that some counties may have no commercial options.
Physician Specialists Gain More Opportunities for Medicare Bonus Payments Tied to Quality
The number of CMS-approved QCDRs tied to payment grows by more than 60% in 2017.

Health Plans Are Actively Exploring Outcomes-Based Contracts
Avalere experts say use of outcomes-based contracts could further goals to improve patient outcomes and manage drug costs
Per Capita Caps Could Reduce Funding for Children Covered by Medicaid
All 50 states and DC would receive fewer Medicaid dollars for non-disabled children.
AHCA Will Remove Low Cost-Sharing Guarantees for Low-Income Individuals
The elimination of cost-sharing reductions could lead to low-income individuals facing higher deductibles and maximum out-of-pockets.
Avalere and FasterCures Release Patient-Perspective Value Framework to Incorporate Patient Preferences into Healthcare Treatment Decisions
Today, Avalere and FasterCures published Version 1.0 of the Patient-Perspective Value Framework (PPVF).
Medicare Advantage Patients Less Likely to Use Post-Acute Care
New analysis from Avalere finds that Medicare Advantage (MA) patients use fewer post-acute care services after being discharged from the hospital compared to traditional Medicare fee-for-service (FFS) patients.

Proposed High-Risk Pool Funding Likely Insufficient to Cover Insurance Needs for Individuals with Pre-Existing Conditions
Funding earmarked for high risk pools in the American Health Care Act will cover five percent of the total number of enrollees with pre-existing chronic conditions in the individual market today.
Avalere Panel Highlights the Importance of Analytics in Value-Based Care
At the Asembia Specialty Pharmacy Summit 2017, an Avalere-led panel identified three focus areas for specialty pharmacies looking to achieve market leadership in an increasingly value-based care environment.
Avalere Deepens Expertise in Medicare Advantage Payment Systems with Hire of Sean Creighton
Sean Creighton has joined the Avalere team as a vice president in the policy practice, and will be responsible for leading advisory services work tied to Medicare Advantage, risk adjustment, and related issues.
Medicaid Per Capita Caps Could Cut Funding for Dual-Eligible Beneficiaries
Capping Medicaid funding could also shift costs to Medicare

Hidden Epidemic of Older Adult Malnutrition: New National Blueprint Advances Integrated Solutions
Citing alarming statistics that show that nearly 1 of every 2 older Americans is at risk of malnutrition and that disease-associated malnutrition in older adults is estimated to cost $51.3 billion annually, a broad group of advocates laid out a roadmap for a new national effort to help millions of Americans who suffer from malnutrition or could be at risk as they grow older.




